#67 Dr. Ashley Mason on Sauna Use for Depression, Conquering Insomnia, and Mindfully Breaking Bad Habits
This episode is available in a convenient podcast format.
These episodes make great companion listening for a long drive.
The BDNF Protocol Guide
An essential checklist for cognitive longevity — filled with specific exercise, heat stress, and omega-3 protocols for boosting BDNF. Enter your email, and we'll deliver it straight to your inbox.
Dr. Ashley Mason is a clinical psychologist and director of the Sleep, Eating, and Affect Laboratory at the Osher Center for Integrative Medicine at UCSF. Her research centers on nonpharmacological treatments for depression, insomnia, and overeating.
In this interview, Dr. Mason and I discuss…
- How clinical whole-body hyperthermia (WBH) differs from ordinary sauna use.
- The strange somewhat suggestive theme of thermoregulatory dysfunction and changes as a component of depression and its treatments.
- How aerobic exercise can improve depressive symptoms.
- The exciting new investigation being lead by Dr. Mason that will interrogate the antidepressant effects and biological changes accompanying eight sessions of whole-body hyperthermia in combination with cognitive behavioral therapy. Learn more about this study which is now recruiting at UCSF in San Francisco.
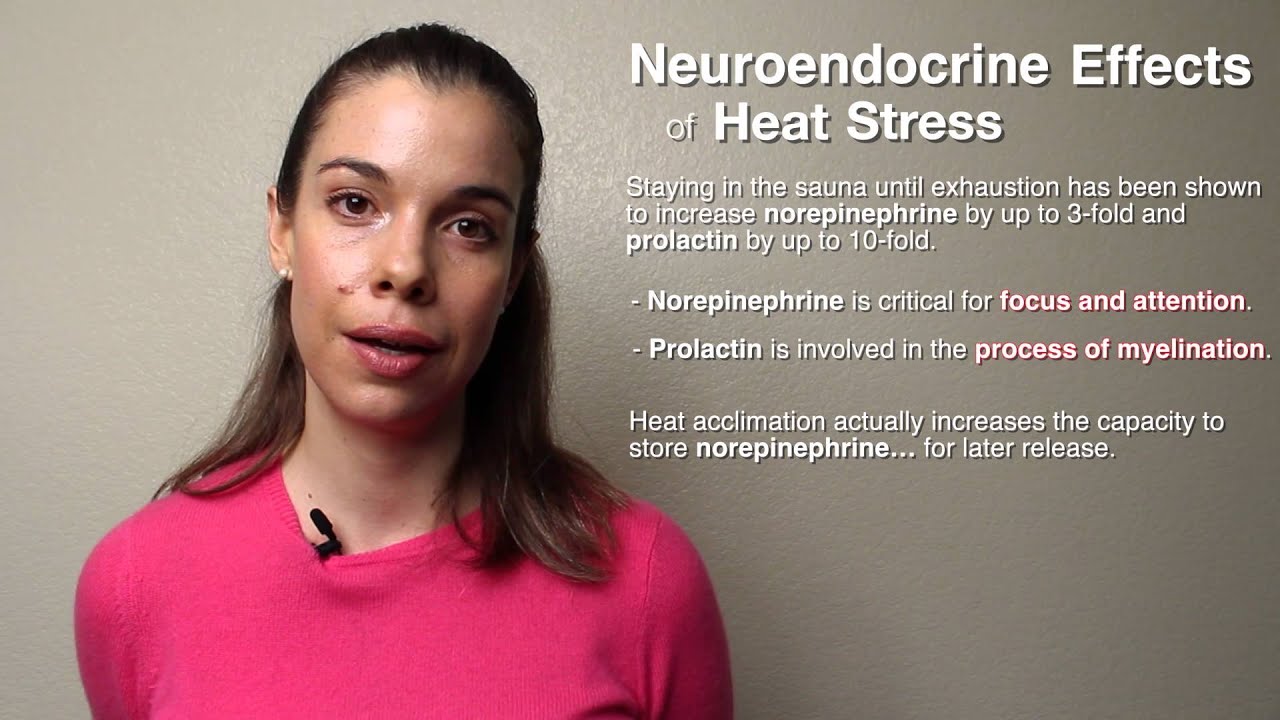
- How the new sauna study will also be interrogating biomarkers thought to be implicated in adaptive responses to heat stress and exercise.
- How sauna use may eventually become an adjunct to clinical whole-body hyperthermia treatments, potentially bridging the gap between more intensive clinical protocols and ordinary home use.
- How having insomnia differs from being a "night owl."
- How cognitive behavioral therapy techniques like sleep restriction, muscle relaxation, and stimulus control can be used to treat insomnia.
Depression has far-reaching effects on a person's physical and social health
Depression is a crippling disorder that affects the lives of roughly 322 million people – more than 4 percent of the global population. It's the most common mental health condition worldwide. People who have depression often experience profound sadness, fatigue, and the loss of interest in things that once were enjoyable, enduring far-reaching effects on their physical and social health.
The first line of treatment for depression is often psychotherapy in conjunction with antidepressant drugs, typically selective serotonin reuptake inhibitors, or SSRIs. But the response to SSRI treatment is moderate at best, ranging from 40 to 60 percent, and roughly one-half to two-thirds of people taking SSRIs don't experience any relief from their depressive symptoms.
Hyperthermia may reduce symptoms of depression
"How can we develop something that could be taken out of the hospital and maybe…transitioned into someone's home? And how can we make this more affordable? There's enough health care that's unaffordable, let's not add to that list." - Dr. Ashley Mason Click To Tweet
Dr. Ashley Mason is investigating non-pharmaceutical approaches for treating people with depression. Her current work focuses on the use of whole-body hyperthermia to reduce symptoms of depression, piggybacking on earlier research in which a single session of whole-body hyperthermia treatment alleviated participants' depressive symptoms within a week of treatment – an effect that lasted for six weeks post-treatment.
Whole-body hyperthermia is a therapeutic strategy used to treat a variety of medical conditions, including cancer, fibromyalgia, and others. It is typically administered in the clinical setting, employing hot-water blankets, warm-water baths, heating coils, or specialized lamps that emit infrared-A radiation in a confined area or chamber, such as the Heckel HT-3000.
But the term "whole-body hyperthermia" is both informative and misleading. As the name suggests, it induces hyperthermia, a state of elevated core body temperature, to elicit its effects. During treatment, a participant is exposed to a heat source until their core body temperature reaches a desired temperature (usually no higher than 107°F [42°C]) for a duration of 60 minutes or longer. The participants' body temperature, heart rate, oxygen saturation, blood pressure, cardiac function, and respiration rate are closely monitored.
Ironically, many whole-body hyperthermia treatments don't actually expose the whole body to high temperatures. Instead, the head is spared from the heat and often kept cool with ice or cool cloths, prolonging the participant's tolerance to the intense heat. This is important because when it comes to heat exposure and depression, more is better – at least in terms of time. Sessions often start out cool and increase in heat over time before achieving the desired final temperature.
Critical differences separate whole-body hyperthermia and sauna use
Recreational sauna use also induces hyperthermia, but critical differences separate the two practices. Typically, traditional sauna sessions are shorter (about 15 to 20 minutes, on average) and might be interspersed with periods of cooling. They usually expose the entire body to heat and only raise core body temperature to approximately 102.2°F (39°C). Saunas are typically wood-paneled rooms heated by infrared or conventional heaters. However, in recent years, single-person tent-like infrared saunas that spare the head from the high temperature have become popular.
Sweat provides a link to how heat stress benefits mental health
Dr. Mason's first clues that heat stress might influence depressive symptoms came when she searched for similarities between the body's responses to whole-body hyperthermia, sauna use, and SSRIs. A surprising common denominator emerged: sweat.
During heat exposure, half to nearly three-fourths of the body's circulation shifts from the core to the skin to facilitate sweating. In a typical Finnish-style sauna session, for example, a person can expect fluid losses of one or two pounds (0.6 to 1.0 kilograms) per hour. Similar losses would be expected during a whole-body hypothermia session. Strangely, hyperhidrosis – a condition characterized by excessive sweating – affects as many as 20 percent of people taking SSRIs. It's noteworthy that people who have depression often have poor thermoregulatory function and exhibit higher core body temperatures, especially at night. Their bodies simply aren't as effective at cooling. Heat stress may correct thermoregulatory function.
Inflammation as a driver of depression
People who have depression often have one or more comorbidities – coexisting health conditions – the most common of which is cardiovascular disease. People who have depression are twice as likely to develop cardiovascular disease, and people who experience an acute cardiovascular event are more likely to develop depression. However, like exercise, heat stress challenges the cardiovascular system, to good effect. As the body's core temperature rises, heart rate and cardiac output increase, blood pressure goes up, and sweating ensues. The outcome of these short-term challenges is overall improved cardiorespiratory fitness and health.
A possible driver of the increased comorbidities seen in people with depression is inflammation. Inflammation is an important component of the body's immune response, but chronic low-grade inflammation drives many chronic disease processes and can promote changes in brain and neuroendocrine function and the development of depressive symptoms. For example, Interleukin-6 (IL-6) is a pro-inflammatory cytokine. Short-term elevation of IL-6 is generally considered favorable, but chronic elevation is indicative of chronic inflammation.
Interestingly, IL-6 also demonstrates anti-inflammatory properties because it switches on the activity of interleukin-10 (IL-10), a potent anti-inflammatory cytokine. People who have depression tend to have elevated inflammatory markers. Exercise and sauna use, both of which elevate core body temperature, acutely increase IL-6 and IL-10 plasma levels and IL-10 expression levels. Dr. Mason, in collaboration with previous FoundMyFitness guest Dr. Charles Raison, Dr. Rhonda Patrick, and others, will investigate the effects that sauna use has on depression, with specific emphasis on assessing the effects of heat stress on inflammatory biomarkers.
Sauna use can provide a means to socially connect
"If whole-body hyperthermia is making people want to talk more, and one of the major reasons why people don't do well in therapy is that they don't want to talk and engage, could using heat cause people to be more engaged in therapy?" - Dr. Ashley Mason Click To Tweet
An often-overlooked aspect of sauna use is the communal nature of many traditional forms of heat exposure. Warming the body to make a person feel better is not a novel concept. The benefits of heat have been recognized for thousands of years. Many cultures observe some form of heat exposure for purification, cleansing, or healing, often in a communal setting, where families, friends, and even strangers gather to share in the healthful practice and connect with others. Dr. Mason has observed that many of the participants in previous whole-body hyperthermia research begin talking while they're receiving the heat treatment – a critical step in engaging in psychotherapy.
Cognitive behavior techniques are beneficial for insomnia and overeating
"Changes in relationship status, a breakup, losing a job, having a kid, raising a kid. There's a lot of different things that can cause insomnia. However, things that maintain insomnia are generally not the same things as what cause insomnia." - Dr. Ashley Mason Click To Tweet
Dr. Mason's other work addresses a growing public health problem: insomnia. Defined as persistent difficulty in falling and/or staying asleep, insomnia is common among older adults, women, and people who have physical or mental illnesses. Estimates of the global prevalence of insomnia vary, ranging from as low as 10 percent to as high as 60 percent. People with insomnia often experience depression, poor work performance, car accidents, and overall poor quality of life. It's no surprise that many people who have insomnia turn to sleeping pills for relief.
But sleeping pills carry many health risks and don't promote quality, healthful sleep. Since a driving force in the development of insomnia is change, especially change that affects relationships, employment, or family dynamics, Dr. Mason employs cognitive behavior techniques that help her patients identify what those changes are and develop strategies that promote, rather than hinder, sleep. These strategies include good sleep hygiene, stimulus control, and sleep restriction – which differs from sleep deprivation. Developing these sleep-promoting behaviors can help reduce dependence on sleeping pills.
Not everyone who has difficulty falling asleep has insomnia, however. What time of day a person falls asleep is dictated by their chronotype – their innate tendency to sleep at a particular time during a 24-hour period. Chronotypes are based on circadian rhythms and are genetically determined. Disruption of a person’s innate schedule can influence mood, productivity, and disease risk. Dr. Mason explains that people who tend to fall asleep and rise later – often called "night owls" – face challenges in a 9-to-5 world that favors early-rising "larks."
"Really slowing down and getting curious about how your body feels and what your experience of the [food] actually is can help you consume less."- Dr. Ashley Mason Click To Tweet
Cognitive behavior therapy also benefits people who overeat. Eating is essential for survival, and hunger is a powerful motivator for food-seeking behavior. But many eating behaviors are rooted in reward-based processes. Consequently, people often eat in response to various non-hunger-related triggers, including emotional or mental stress or external prompts, such as advertising and social pressures. Dr. Mason's approach helps people who overeat become more mindful of the triggers that drive them to overeat. Mindfulness helps reward-based eaters recognize habits that undermine healthy eating patterns and behaviors and moderate intake.
Learn more about Dr. Ashley Mason
- Learn more about the HEAT BED Study - currently recruiting!
- Sleep, Eating, and Affect Lab
- UCSF Profile
- @DrAshleyMason on Twitter
- Google Scholar Profile
Relevant publications
- Feasibility and acceptability of a Whole-Body hyperthermia (WBH) protocol
- Whole-Body Hyperthermia for the Treatment of Major Depressive Disorder
- Cytokines sing the blues: inflammation and the pathogenesis of depression
- Can Mindfulness Address Maladaptive Eating Behaviors? Why Traditional Diet Plans Fail and How New Mechanistic Insights May Lead to Novel Interventions
- Sauna use as a lifestyle practice to extend healthspan
Relevant episodes
- Dr. Charles Raison on Depression, the Immune-Brain Interface & Whole-Body Hyperthermia
- Exercise as a Treatment for Depression
- Cognitive behavioral therapy for insomnia (CBTI) as an alternative to sleeping pills
- The Underlying Mechanisms of Depression
People mentioned
-
How clinical whole-body hyperthermia (WBH) differs from ordinary sauna use.
-
-
The strange somewhat suggestive theme of thermoregulatory dysfunction and changes as a component of depression and its treatments. 1
-
How chronic inflammation plays a critical role in some forms of depression – but sauna use may reduce it. 1
-
How lipopolysaccharide injection induces depression symptoms, but high-dose EPA (an omega-3) ameliorates them. 1
-
How aerobic exercise can improve depressive symptoms. 1
-
CBT+Hyperthermia trial. The exciting new investigation being lead by Dr. Mason that will interrogate the antidepressant effects and biological changes accompanying eight sessions of whole-body hyperthermia in combination with cognitive behavioral therapy. Now recruiting at UCSF in San Francisco.
-
How heating the body more slowly and with greater intensity may be an important component of the effectiveness of whole-body hyperthermia.
-
How the new sauna study will also be interrogating biomarkers thought to be implicated in adaptive responses to heat stress and exercise.
-
How sauna bathing and similar practices often provide opportunities for people to connect socially and why this may be an interesting corollary when viewing it through a therapeutic lens.
-
How sauna use may eventually become an adjunct to clinical whole-body hyperthermia treatments, potentially bridging the gap between more intensive clinical protocols and ordinary home use.
-
How hyperthermic baths (40°C) may also be an approach to eliciting antidepressant effects, according to a randomized clinical trial. 1
-
How having insomnia differs from being a "night owl."
-
How cognitive behavioral therapy techniques like sleep restriction, muscle relaxation, and stimulus control can be used to treat insomnia.
-
How to learn to use CBTi techniques on your own through a book recommended by Dr. Mason, called Quiet Your Mind & Get To Sleep.
-
How cognitive behavioral techniques and smart, extremely conservative dose reduction can prevent rebound insomnia when weaning off prescription sleep medication under the guidance of a prescriber.
-
How cognitive behavioral therapy can help people break bad habits, including eating behaviors that harm health. 1
-
How a technique called motivational interviewing can help reduce sugar-sweetened beverage consumption.
-
How visualizing near-future health goals helps people make better decisions "in the moment."
Dr. Patrick: Hello everyone. I'm sitting here with Dr. Ashley Mason, who is the director of the Sleep, Eating, and Affect Laboratory at the Osher Center for Integrative Medicine at UCSF. I'm super excited to have her here today. She specializes in various different non-pharmacological treatments for changing behaviors, I guess, whether that's sleep or eating behavior disorders, or affect disorder. So mood disorders. And I've had two of your former mentors on the podcast, Dr. Elissa Epel, who I believe was your postdoctoral advisor at UCSF, and your former graduate advisor, Dr. Charles Raison, who...
Dr. Mason: One of them.
Dr. Patrick: ...one of my favorite podcast guests, who's done a phenomenal job on starting this whole body of research on the effects of whole-body hyperthermia for treating affect disorders like mood disorders and depression. And so I'm super excited to dive into all that with you today. But maybe we can start with some of our overlapping passions with getting hot.
Dr. Mason: Absolutely, absolutely. Well, thank you so much for having me here today. Long-time fan of the show. It's really exciting to be sitting here with you. And yes, I'm super passionate about sauna and whole-body hyperthermia protocols and their entry into the space of treating mental health disorders. I think it's a really exciting area.
Dr. Patrick: So maybe you could refresh, you know, the viewers' or listeners' memory, or even people that are not familiar with the podcast we had with Dr. Charles Raison where he discussed... People are familiar with the term sauna and they know, you know, a lot of people use the sauna, or they've, you know, seen it at their gym. But whole-body hyperthermia is a new term for a lot of people, and it's a really important one because that is what, you know, clinically was used or is used to treat, or shown to help treat depression. Can you explain the nuance there with whole-body hyperthermia and how that's different from just going in the sauna?
Dr. Mason: Sure, sure. So it's an emerging field. And, like you said, a lot of people are familiar with sauna. It's at their gym, it's maybe even in their house, it's when they go on vacation. And going in the sauna and sweating and then leaving it is very pleasurable. It is often relaxing, calming. People enjoy doing it. They often report that they feel better afterward. Whole-body hyperthermia protocols are a little bit more intense. So if you ask someone who went into one of the saunas, in one of the studies that I'm sure we're going to talk about today, they might just not tell you it was a spa-like experience. It's very intense, there's a lot of sweating, and you get very, very hot. And, whereas with sauna, you might go in it for 15, 20 minutes, go out of the sauna to cool down for a bit, go back in. With whole-body hyperthermia protocols, you're getting heated pretty consistently for quite a while until you're on the other side and you're going to be done. It's not so much a going in and going out and going in process. And with whole-body hyperthermia protocols, especially in studies, there have been a lot more steps to control the experience than, say, going to a sauna at your gym. We can get into what some of those are if we want to talk about the specific studies. But they're pretty different experiences, although they both involve heat.
Dr. Patrick: And maybe, like, let's talk a little bit about some of the preliminary findings that got you interested in this research in the first place.
Dr. Mason: Yeah, absolutely. So in 2016, this paper came out by Janssen and a bunch of other co-authors where they reported on a whole-body hyperthermia protocol that they had used to test as a treatment for clinical depression. And this study was impressive for a number of reasons. They recruited 30-some-odd participants who had pretty significant depression. And they randomized half of them to get a whole-body hyperthermia treatment, or half of them to get a sham whole-body hyperthermia treatment. And I'm going to talk about what the differences are there in a second. But it was a very good idea for a placebo condition for this study. So the whole body hyperthermia condition, the folks randomized to receive this were put into a kind of whole-body hyperthermia machine that involved infrared heating lamps. And this is a pretty fancy machine. They run about $50,000. You only find them in hospitals. They're made in Germany. It's called a Heckel. And it's a pretty involved experience. So these people who were randomized to receive whole-body hyperthermia went into this sauna tent, if you will, the Heckel machine, and they were heated until they reached a core body temperature of 38.5 degrees Celsius. After that time, the sauna was turned off, and they stayed in there anyway for another hour just lying there. And during that time, their temperature actually continued to rise all the way up to about 38.85 or so degrees Celsius. And all during that time, they are sweating, sweating, sweating. They're hot. And what's really important to know about the sauna tent is that their head is outside of the sauna. So you asked about the differences between regular sauna and whole-body hyperthermia, this is a major one. When you go into a sauna, your whole body is going into the sauna, including your head. With these whole-body hyperthermia protocols, in many cases, your head is not in the heating element, it's outside of it. So you can be drinking, a person can be attending to your head, putting cool cloths on it, and so on, like they did in that Janssen study. Now, the other half of the people who didn't get the whole-body hyperthermia, they were actually put in that same machine, but it wasn't turned on to be very hot. And the lamps turned on, and they got a little bit warm, but they didn't get anywhere near as warm. I think it was like 99.5 degrees Fahrenheit that the control condition got into. And what's more is that the authors of the study actually asked all of the participants, "So what do you think you got? Do you think you got the real deal, the whole-body hyperthermia, or do you think you got the control condition?" Some 71% of people in that control condition thought they got the actual sauna treatment. So why is that exciting? Because when you actually look at the change in the depression scores for these people, it was pretty remarkable. The drops in depression within a week were pretty impressive. And what's more, those drops were maintained six weeks later. And this was one whole-body hyperthermia session. And so the difference between the groups was pretty notable six weeks out, and especially one week out. And this study caught my eye for a few reasons. One is that, as a whole, in this country, in many other countries, we're not just great at treating depression. It's a big problem. Antidepressants work for many people, therapy works for many people, but we still have a long way to go in developing treatments for depression. And when you see a treatment like that, with that strong of a control condition and those effect sizes and those reductions in depression, it catches your eye. So I got really excited about that, started looking more into, "Well, what else has been done with this?" And it turned out there was one other study in 2013, the Hanusch paper where they just recruited depressed participants, they gave them the sauna session, and then they looked at them afterward. And there are some really neat, striking findings about that study as well. But it was a single-arm study, because there was no control condition. But those two studies got me really excited and started me down this path, in particular with looking at temperature.
Dr. Patrick: There was a couple of things you said with, you know, Dr. Charles Raison's study, 2016 study, with this Heckel machine, this whole-body hyperthermia, that are really important. And those are that, one, you said that there was an effect within just a week of treatment, which is quite quickly. It's soon. I mean, like, if you think about classical, like, serotonin reuptake inhibitors, SSRIs, which are used very, you know, widely for, you know, depression treatment, they don't work that quick, they don't work immediately like that. So that was one thing, to get your thoughts. And, two, the fact that they did one session and it lasted six weeks. Like, they didn't have to keep going every day or even every week. I mean, they just did it once, and it was a six-week...like, there was a lasting effect. So what are your thoughts on...?
Dr. Mason: It was a big moment for me. And what I realized when I was thinking about that very SSRI thing was that, "Well, wait a minute, what do SSRIs have in common with all of this?" And I went back and I looked at some of the SSRI literature, and it turns out that one of the most common side effects of SSRIs is hyperhidrosis, it's sweating. So then I thought, "Huh, sweating one of the most common side effects of SSRIs. And yet, with whole-body hyperthermia, what are we actually doing? We should probably actually go back into some of the mechanisms a little bit here with this." But that really made me think, "Okay, wait a minute, do we have actual data now? Has anybody published on whether sweating in response to SSRIs is associated with if they're effective or not?" I'm actually not aware of a paper that has done that. It'd be a great paper and a great analysis to do. I hope someone is working on it. I'd love to work on it. There's a lot of data that we could use to test that. But getting back to your question about, wow, this works really fast. Yeah, SSRIs take weeks, can take months before they start to work, whereas Dr. Raison noticed these effects in just a week in his study design. And yes, they did last out to six weeks, and they didn't measure beyond six weeks. So we don't know what happened, and that's a key area of future research. But maybe we should talk a little bit about the hypothesis underlying why this might be working. And that's where my mind went after I saw that 2016 paper. I thought, "My goodness, what's going on here?" Well, it turns out there is literature showing temperature dysregulation in people with depression. Back early 1982 and then '97, a researcher, Dr. Avery published some work showing that people with depression often have higher nighttime body temperatures, and they're not as good at thermoregulatory cooling. They don't sweat as much to cool themselves down. And what's also been interesting is that there's other work that shows that when people with depression get better, when their depression symptoms lessen, their core body temperature also can decrease. And that's in the context of other treatments that aren't related to sauna treatment, for example, electroconvulsive therapy, ECT. There was a paper that showed that with successful ECT treatment, the patient's temperatures dropped alongside their depression. And from that Hanusch paper, that single-arm sauna trial, what they found was that the decrease in body temperature was correlated with a decrease in depression. And they measured that decrease in body temperature pretty carefully. They were using an indwelling rectal probe. So they were really measuring it those five days afterward, and that says something about the mechanism here with body temperature.
Dr. Patrick: And thermoregulation, perhaps, somehow, sauna use changing the thermoregulatory...
Dr. Mason: Turning it on, possibly.
Dr. Patrick: ...system somehow.
Dr. Mason: Yeah, yeah.
Dr. Patrick: Now, this is a...when you were talking about, you know, clinically depressed people, you know, most people experience depressive symptoms in their lives because of events that happen, maybe a death of a loved one, or stress from work, or financial stress, or relationship stress. I mean, there's a lot of life experiences that can cause, you know, like, people to be sad. But you're talking about something different here, right? You're talking about a clinical type of depression, which isn't just, you know, feeling sad, you know, or anxious because of a certain experience. You're talking about...
Dr. Mason: Right. Being depressed or down most of the day, nearly every day, for quite a few days. This is major depressive disorder, so it's an actual mental health disorder.
Dr. Patrick: Right. And those people, like you were saying, there's a correlation between not regulating the body temperature, correctly and that type of [crosstalk 00:13:26.549].
Dr. Mason: In some studies, there are...some samples...and, again, these are small samples, but what the researchers have found is that these patients' body temperatures are higher and that when their depression symptoms improve, the body temperatures decrease. So there's something there. And also that these people's body temperatures just tend to run hotter than other non-depressed samples.
Dr. Patrick: Do you know if...this is off-topic, but do you know if stress itself or stress hormones, or, you know, something there changes the thermoregulatory system? So, for example, if someone were to have, like, some sort of serious stress, like death of a loved one or something, and the stress, do you think that could possibly cause dysregulation of that system? Is there...?
Dr. Mason: I can't speak...
Dr. Patrick: Is that off the wall question, kind of?
Dr. Mason: I can't speak to the data, because I don't know the data on that. But it seems plausible that if we become really distressed and start to experience some of the symptoms that people with major depressive disorder are experiencing, and we're experiencing them, and it's somewhat of a prolonged way, that we could develop that. But we just don't have the data right now. There's a lot of depression that is situational, as you described, a lot. But there's also depression that's biological. And so we don't know so much which camp that's falling into.
Dr. Patrick: Right. I think another plausible mechanism...I know Chuck and I, or Dr. Charles Raison and I discussed this, and you and I as well in conversations that we've had. But inflammation...and this, I know, like, there are studies that have shown you can take a healthy individual who is not known to have any sort of clinical depression, and you can inject them with lipopolysaccharide, which is, you know, a piece of the outer membrane of bacteria, and it causes a very potent inflammatory response in humans. You inject them with the lipopolysaccharide, and they have an inflammatory response. They have activation of their immune system. The body's like, "Oh, bacteria. I got to fight it off. I don't want to get sick." So inflammation is generated. And, as you know, and we've talked about a lot in the podcast, you know, inflammatory molecules cross over the blood-brain barrier, and they disrupt neurotransmission in there, all sorts of things happening, you know, microglial activation. And what's been shown is that people experience...healthy people experience depressive symptoms after being injected with this lipopolysaccharide, versus a saline control. So people, individuals that were injected with saltwater, didn't have those depressive symptoms when they did some sort of questionnaire or scale, which you're familiar with, probably, but not me. But what was interesting is that, in addition to that, people were given a high dose of EPA, which is one of the marine omega-3 fatty acids that's very potent at negating inflammation. And the people that were given that and injected with lipopolysaccharide didn't experience the depressive symptoms. What I'm getting at here is that, you know, it seems as though that study itself...and there's actually is more than one that showed this. You could cause or induce depressive symptoms in healthy individuals just by causing inflammation. And you could prevent that by giving someone "something that's anti-inflammatory." Which I thought was so impressive and amazing and important because, you know, inflammation, there's so many sources of inflammation. So many different lifestyle factors, obviously, you know, sickness. I mean, people do feel depressed when they're sick, too. But the sauna and inflammation and how the sauna affects inflammation is a whole other interesting area, and particularly because, you know, we know for a fact that...lifestyle factors that can improve depression. And, you know, your specialty is non-pharmacological treatments. You know, of course, exercise is one of the big ones, right? I mean, exercise has been shown in multiple studies to help improve depressive symptoms in people with, you know, major depressive disorder or have clinical depression. And, of course, it's not easy to get someone who's depressed to exercise. But the fact of the matter is that it does work, in some cases, not all the time, but it does work. And the sauna, and there's many different ways that the sauna does mimic cardiovascular...moderate cardiovascular exercise. We have a lot of the same physiological responses, the increase in blood flow to the skin, the sweating to cool down the core body temperature, which increases with aerobic exercise. It also increases with sauna. Elevated heart rate, you know, blood pressure changes, the blood pressure increases while you're exercising or while you're in the sauna, then afterwards, it goes down even below baseline level, so lots of different similarities. And, of course, there's been head-to-head comparisons comparing moderate aerobic exercise to sauna use. So there's definitely some overlap there. So, you know, what are your thoughts on, like, well, maybe this is also helping depression in a similar way that exercise or specifically cardiovascular exercise would?
Dr. Mason: Yeah, absolutely. I think the pathway is totally plausible. But you hit the nail on the head. A lot of times, we would love it if we could get people with depression to exercise. But that is just too much to ask, in a lot of cases. It's also the case that not everybody can necessarily just go and exercise. I know that sounds a little bit crazy, but there are actually lots of people who have injuries or other problems that prevent them from engaging in the kind of exercise they would need to do to have that antidepressant effect, which is aerobic exercise, right? I think running is one of the most well-looked at ones, and it works well for mild and moderate depression. Remember, a bunch of these studies have divided out the depression by mild, moderate, and severe to look at which ones exercise works for best. And I don't quite recall off the top of my head at this moment which it was the best for. But getting people with mild depression to exercise, I think, is much more feasible than getting people with severe depression to exercise. But if we're able to actually capitalize on sauna, if people are more open to using whole-body heating practices, then maybe we have an avenue in to get at some of those biological pathways that exercise is triggering, like you just described. And that's why I think it's really important to start measuring those pathways in whole-body hyperthermia studies. And I'm not aware of any whole-body hyperthermia study looking at depression as an outcome that has measured those. So that's on our to-do list.
Dr. Patrick: Right. Yeah. I mean, that's something... So you've got a couple of studies one that's probably like...it was like a proof-of-principle-that-it's-safe study.
Dr. Mason: Yeah, yeah. It's under review right now. We did a study...right before COVID struck, we finished up this 25-person study to develop the protocol that we're going to be using at UCSF for our future trials.
Dr. Patrick: Maybe you can talk about why. So you talked about this Heckel machine, and it's very expensive, and it's, you know, made in Germany, but that's not what you're using.
Dr. Mason: No.
Dr. Patrick: So maybe we can talk about what you're using and why and your personal story about how you came to figure that out, because it's pretty funny.
Dr. Mason: It's a pretty funny one. So after that paper in 2016 came out and I got all excited about the study, and I emailed Chuck, or Dr. Charles Raison, about it and started talking about, how could we do this research? Well, it turned out it was actually really difficult to do research with that machine without a lot of money and without a lot of resources. And at the time, I was pretty junior at UCSF. I had just become an assistant professor, just gotten my first big NIH grant and wanted to figure out, well, how can we do this? And not only can how can we do this in a way that's feasible in science, but how can we actually develop something that could be taken out of the hospital that is actually more accessible, that might even someday be able to be in all kinds of settings, not just hospitals, maybe something that could be transitioned into someone's home? And how can we make this more affordable? There's enough health care that's unaffordable, let's not add to that list. So I decided to see what I could do, and gathered a group of friends and said, "Hey, guys, we need to go and figure out if we can find a sauna that can get our core body temperature up as hot as this machine can." So I went to Walgreens and bought a whole bunch of thermometers, handed them out and said, "All right guys, here's the list of all the different places to go and try these different saunas." And there was a Russian banya, there were a bunch of health spas, there were some other spas that have started having these infrared saunas. I have some friends who had infrared saunas in their house by that time. And everybody just started doing a bunch of testing for me. And we learned really quickly that man can't get to that core body temperature, because you can't stand to stay in that long. In these protocols, the Janssen protocol and the Hanusch protocol, people were in the sauna for well over an hour...two hours, in the Hanusch case, and I think 107 minutes on average in the Janssen paper. That's a long time to be in that little device.
Dr. Patrick: You'll never be in a 179-degree-Fahrenheit sauna for that long.
Dr. Mason: No.
Dr. Patrick: Absolutely impossible.
Dr. Mason: Absolutely not.
Dr. Patrick: You shouldn't it would be detrimental to your health.
Dr. Mason: Very dangerous, bad idea.
Dr. Patrick: So you were going around sticking thermometers in your butt...rectal, right?
Dr. Mason: Definitely, that's what everybody was doing.
Dr. Patrick: So that's the most accurate way to measure core body temperature.
Dr. Mason: Best way.
Dr. Patrick: And what increase in core body temperature? Was it a two, or two and a half? What was the degree?
Dr. Mason: Yeah, looking for about...on average, if people run their baseline between 97 and 99, right, a 2-degree temperature change could mean a lot of things for different people. So I was really looking to see, could people get to 101.3, because that was the temperature in the Janssen and Hanusch protocols. And it turns out the overwhelming answer was, well, no.
Dr. Patrick: What about the 20 minutes at 190? Where does that get you, 190 Fahrenheit?
Dr. Mason: I don't know. There was only...
Dr. Patrick: That's my typical sauna.
Dr. Mason: There was only one place, I think, that we could find that had a sauna that hot, and that was a Russian banya in San Francisco. All the infrared ones don't get that hot, actually. And so...
Dr. Patrick: Yeah, no infrared definitely was like 140?
Dr. Mason: They don't. One forty to 160 I think...
Dr. Patrick: One sixty, okay.
Dr. Mason: ...you can get up there. There's a bunch of variability, though. So, anyway, ultimately, I only ever had a couple of friends who were able to get that hot maybe once or twice. And they said it was relatively excruciating. They thought they were going to faint. Like, you know, the descriptions that they gave me would never have passed through the Institutional Review Board at UCSF. And I thought, "What am I missing here? What's the key detail?" But it turns out that key detail is having your head out of the sauna. So then we rebooted and started looking around for heating devices where your head is not inside of it. And, behold, found one of these sauna domes. And got a few of those, started testing that out. And it turns out, you can stand to be in that thing for a lot longer than to be in...
Dr. Patrick: So this is an infrared sauna dome, head out.
Dr. Mason: Head out.
Dr. Patrick: And it's like something you can just buy on Amazon or something.
Dr. Mason: You can buy one on the internet. There are so many kinds. Now, obviously, we had to pick a kind and then had to do...we had to apply for something called a nonsignificant risk determination through the UCSF IRB in order to be able to use it. I had to write up a whole protocol, say what I was going to do, say how it was going to work, how I was going to keep people safe, all of these things. They had to review it. It took about a year to get the approvals to do that one first study. And you might be wondering, "Well, okay, so people are lying in this tube..." Doctor Raison sent me his Mindray rectal probe machine that I could use for the study, which is a rectal probe that's in there the whole time. It's silicone. It's not a big deal. And no one in the study that I did with 25 people had any complaints or anything about it. As soon as they saw it, they said, "Oh, that's not a thing. I can put that there." And it was no big deal. And in order to keep people able to stand this for that long, we developed a whole protocol where a person sits at the head of the person who's in the sauna and is giving them water when they're thirsty. And, most importantly, is using giant ice cubes and cold cloths all over their head to keep them cool in their head. And it's remarkable what a difference this makes and what a role it plays. And it helps people stay calm, it helps them stay comfortable. Because we did some test runs with folks with and, you know, without it as much, and people were overwhelmingly more comfortable when they had ice on their face. Turns out, you do this protocol, people can stay in the sauna. It takes about 70 to 80 minutes. It was comparable to the protocols from the Janssen and Hanusch papers. And we were off to the races. So we did it with 25 people, and those data are under review now.
Dr. Patrick: What temperature was it, the dome?
Dr. Mason: It was about...gosh, it's hard to say. I think it was about between 144 and 150-ish. It was not as hot as you would think.
Dr. Patrick: And it was on the entire 80 minutes?
Dr. Mason: And so that's another really important thing. So I think there's a whole category of things we've discovered from the existing literature. And one of the really important ones is that the time that you are taking to get to that temperature also might really matter. When people got into those sauna tents in those two other studies, they were cold. And then the researchers turned them on and heated them up. And so that's what we did in our study as well. They got in, we turned it on, and then they heated up as the ambient air heated up. And in a recent paper that, actually, incidentally, Janssen and Hanusch had written together, they reviewed some of the studies that exist for looking at whole-body hyperthermia for depression. And one of the things they noted is that the effect sizes of the change in depression from before to after the intervention, in other words, the size of the reduction in depression, was higher if people spent more time getting to that peak temperature. So longer seemed to be better. And, in hindsight, that's not really rocket science. I mean, it makes a lot of sense. If you take a frog and you throw it into boiling water, it jumps right out, because it says, "This is too hot, I can't stand this." But if you put the frog in the cold water, and then you slowly heat it up, it can stand to be in the heat for a whole lot longer. And it's going to get much more of the effects than the brief amount of time it was in the boiling water. So this paradigm where we start people cool might have multiple effects. One, it might help people actually be able to endure this treatment better. Because if you and I are thinking...oh, getting into our 190-degree Finnish sauna, like, it's hot, the minute you get in you are going. But these people don't start with that shock. They're just like, "Okay, I'm lying here. It's getting warm. It's getting warmer." And maybe it helps them withstand it and be able to do it longer. Because, as I said, it's not a spa treatment. It's not a walk in the park. It's intense. And so, I don't know exactly where we started with that, but I got all excited about how this protocol is working.
Dr. Patrick: What's interesting, though, also, because you mentioned, like, for example, I get into this 190-degree, you know, Fahrenheit degree sauna, and I want that thing hot when I get in. I don't want to waste my time, you know. [inaudible 00:29:18] be hot. I'm going to get in there. I'm going to sweat. But I'm also heat adapted. And, you know, there have been studies showing that, you know, the more you expose yourself to heat, whether...or the more you elevate your core body temperature, which can be through, you know, ambient heat, so like a sauna, or a hot bath, or a steam shower or...
Dr. Mason: Exercise.
Dr. Patrick: ...yoga or exercise, the more adapted you become. So your body starts to sweat at a lower core body temperature to cool yourself down. All these other physiological changes start to happen. Your heart rate variability, you know, improves. All those things happen when you're adapted. And when you're adapted, it becomes easier. It's like, "Oh, I'm sweating at a lower core body temperature, so I'm feeling cooler, and I can stay in easier," right? And also heat shock proteins. We'll talk about biomarkers for heat shock proteins, which are proteins that are, you know, classically known to be involved with...you know, they're stress response proteins. So heat is a form of stress, and they get activated with many types of stress, but heat is one of them. And they basically protect proteins inside of your cells from aggregating and becoming misfolded and forming plaques and disrupting things. They also help prevent muscle atrophy. They play a role in preventing your muscles from atrophying. And they play a lot of neuroprotective roles and neurodegenerative...they do a lot of things. But they also kind of help your body deal with the heat stress, and this is part of the adaptation. And so people with, like, higher levels of heat shock proteins, so people that are heat adapted, they increase their heat shock proteins upon exposure to heat sooner than people that are not adapted. And so, kind of, what you're saying makes sense where you're not just shocking them all at once, but they might be slowly adapting in a way, you know, like, on a physiological level.
Dr. Mason: It could be, and it's their first time, so it's very new. They're not adapted in any way to that yet.
Dr. Patrick: Totally. I've noticed, like, with, for example, my mom, who...boy, she can sweat at, like, the minutest little temperature change where she's like, "It's hot here. Where's my fan?" you know? So I've been getting her in our sauna, and the first time she got in, it was like five minutes. And I did it at 165, which is typically what a lot of gyms are at, 165 Fahrenheit. She was like, "I couldn't..." She couldn't stand it for more than five minutes. And I said, "That's okay. It's your first time, you know." And then the second time she did it, she was in there less than 10, but it was more than 5, you know. And then now she's like, you know...I mean, she can stay in there 10. But sometimes what she'll do is she'll stay in there for 10 and then get out. She'll get on the lower bench. She'll get out for a couple of minutes and then come back in. But the first couple of times, it was like, "I can't do this. This is too much," you know, "for me."
Dr. Mason: That's why it's so important to develop these protocols in ways that people will actually do them. Because as much as we wish, you know, we could have people do all kinds of things, exercise or eat certain things. If people won't do it, then it won't work.
Dr. Patrick: Right. Yeah. And you mentioned this also, which is a very important point, is there are a lot of disabled people. Like, there are people that can't go for a run, whether it's joint injuries or something more severe. I mean, there are people that can't do, like, aerobic exercise. And there are also people that have never done it in their entire life, and they're older. And it's like, good luck getting someone who's never been physically active to, like, start being physically active in their six-decade of life. It's really hard. So the sauna, it's not only, like, you know, more applicable in the sense that people are more compliant, because it's easier to go sit in something than it is to go for a run. But, I mean, people that can't go for a run, like, physically, that's amazing, right? I mean, being able to do that.
Dr. Mason: And I think that's where this comes in, too, for thinking about cardiovascular disease, which I know you've thought a ton about, and you gave that talk about, and, you know, it's a big theme. And one of the things we should definitely mention is that cardiovascular disease and depression, those often happen together. And so there's a large group of people who are struggling with cardiovascular problems, and also depression, for whom this may be a treatment that could have an effect for both conditions. So one of the other aspects to think about when developing a protocol like this is, can we use it for other conditions too not just mental health, but maybe also other physical health conditions that are affected by exercise and heat?
Dr. Patrick: Right. So let's talk about the...so you're now doing a study.
Dr. Mason: Yes.
Dr. Patrick: Hopefully, you're starting soon. COVID's delayed it a bit. It's delayed much research in the world. But let's not talk about that. So this new study that I'm super excited about, and I get to play a very small role, collaborative role with you.
Dr. Mason: It's going to be so fun.
Dr. Patrick: Let's talk about it. Because biomarkers, which is where I come in with my enthusiasm...
Dr. Mason: Absolutely.
Dr. Patrick: ...and being able to look at, you know, how a sauna may affect people with depression at, you know, like a real molecular level, right?
Dr. Mason: Yeah, in the cells.
Dr. Patrick: Yeah. So let's talk about that study, which hopefully will start very soon.
Dr. Mason: So we're really looking forward to this study. It's going to be a three-year project to do this pair of two studies. The first study will be 16 people, and everybody's going to get the same thing. And I'll talk about what that is in a second. And the second study is going to be 30 people. And half of those people get one thing, and half of those people get another thing. So let's talk about what everybody is getting in the first study. So, first of all, in both these studies, we're going to measure all of those biomarkers. It's going to be pretty exciting. You've mentioned a number of them so far, BDNF, heat shock proteins, inflammatory cytokines, gosh, CRP. There's a little bit of a laundry list we've got going.
Dr. Patrick: So people that don't know what BDNF is, brain-derived neurotrophic factor. And what role does that play in depression, just, like, generally speaking?
Dr. Mason: My goodness. So I'm not up to snuff, I would say, on all of the biological underpinnings with these molecules with depression. But there's...
Dr. Patrick: It's one of the things where exercise has been shown to increase, and it's thought that may help with neuroplasticity.
Dr. Mason: Right. But there's been a whole bunch dating back to Dr. Charles Raison's paper in 2007, called "Cytokines Sing the Blues," looking at how depression may be quite inflammatory for some people who have it. And so we know that exercise is temporarily inflammatory when you do it, but it's actually in a good way because of the adaptive changes that follow from that.
Dr. Patrick: The anti-inflammatory change.
Dr. Mason: Yes, right. So the thought is, well, sauna is hopefully quite similar. And we have a bunch of data that suggests that it is looking in that direction. We still need to do the research, though. So in this first study, we will have 16 people with major depressive disorder. We will recruit them. They will all be adults. And in addition to getting a whole-body hyperthermia treatment, they're also going to get something called cognitive behavioral therapy for depression. So what is that? Cognitive behavioral therapy is a psychotherapy used for depression. It's considered gold standard. It's a first-line treatment for depression. It doesn't involve medications. It's just a therapist who provides this treatment. It's pretty structured. It's pretty standardized. There are very specific tools that are often used across all of the different ways of administering this treatment. But the idea is that thoughts impact our feelings, and how we feel impacts our behavior. So, for example, if you have someone who has, let's say, type II diabetes, and they come in and they say, "I'm never going to be able to get my blood sugar under control. I'm never going to be able to do it. I just can't seem to stick to this diet. I'm always going to fail. I'm never going to be able to do this." When someone has those series of thoughts, how do you think they feel? Not so great. They don't feel so great. And when you don't feel so great what do you do? Well, the chocolate cake sounds pretty good. Maybe I'll eat some chocolate cake to feel better. But then you eat the chocolate cake, which reinforces the thought, "I can't do this. I'm never going to be able to stick to this diet," and so on and so forth. So thoughts, feelings, behavior, thoughts, feelings, behavior. And so interrupting that loop is a major part of cognitive behavioral therapy for depression, and there's a bunch of different ways that that's done. Anyway, this treatment is known to work. However, it doesn't work if people won't do it. And what is one of the major reasons why people with depression can't really get some benefits out of psychotherapy? They can't really engage, because they're super depressed. Notwithstanding, of course, there are huge problems with our medical health care system in terms of being able to get therapy. That's a whole nother can of worms that we don't need to go into. But the point that I'm making is just that if patients can't really engage in therapy, they can't really get the benefits out of therapy. So, in this treatment, everybody's going to get whole-body hyperthermia, as well as cognitive behavioral therapy sessions. Not at the same time. They might be on separate days, or they might be on the same day, but one after the other. And you might be wondering, well, where did this idea come from? Like, why give cognitive behavioral therapy with whole-body hyperthermia? And that dates back to a few different things. And I think you and Dr. Charles Raison talked about this during your discussion about some of the traditional origins of sauna. It's often been a communal process, Native American sweat lodges. People don't go on those by themselves, right? It's a group. Or in the Korean kilns, or in the Russian banyas, right? It's been a social experience. And one thing that Chuck told me about the 2016 paper and about that study was that, during the study, the patients who were getting the whole body hyperthermia often started chatting. I don't remember if you guys talked about this part or not, but...
Dr. Patrick: Just from personal experience, it's absolutely true. I mean, you become chatty when you're in the sauna. And, like, you talk to people when...yeah.
Dr. Mason: Yeah, started wanting to connect, started wanting to...and so the research assistants went back to the investigators and said, "The patients are talking. What should we be saying to them? What should we be doing?" And I remember when Chuck told me this story and just thinking, "Well, if whole-body hyperthermia is making people want to talk more, and one of the major reasons why people don't do well in therapy is that they don't want to talk, and they don't want to engage, should we be pairing these things? Could using heat then cause people to be able to be more engaged in therapy?" And so this is the ultimate mind-body type intervention, right? There's no drugs here. And if we can develop something like this, that gets around prescribing people medications, maybe this is a good way to go. So proposed this dual intervention with a mind and a body component, and that's what we're moving forward with. So we're developing that combined intervention. And then in the second study, with the 30 people, we're randomizing half of people to just get the cognitive behavioral therapy, which we know works. It's in the literature. There's reviews, meta-analyses showing that cognitive behavioral therapy for depression works. Half people will get that and then half will also get the whole body hyperthermia sessions. And we will see, does adding the whole-body hyperthermia lead to larger depression decreases? And you might be wondering, "Well, why don't you do it differently? Why didn't you just do just the sauna versus, like, just CBT or something like this?" Well, it's really tricky ethically to recruit patients with depression and then not provide them with a treatment that we know works. And tell them, "Oh, and by the way, don't do anything else while you're doing this thing." That's a very, very tricky thing to do. The better thing to do is to say, "Okay, here's what we know we have already. Can we do better than that?" One of the key gaps that we're addressing is we're going to be giving people eight weekly whole-body hyperthermia sessions.
Dr. Patrick: Right.
Dr. Mason: So that's a lot. We're going to see, are people willing to do this? Do they get more benefit this way? Because those other two studies that I mentioned, they only gave one whole-body hyperthermia session, and we saw that huge drop one week later. What happens if we give a second session one week later? Are we going to see another huge drop? We don't know. We need those data. So we're going to be doing multiple whole-body hyperthermia sessions. We're also going to be measuring body temperature at night, during their entire time that they're in treatment, because they're going to use a wearable device to do that.
Dr. Patrick: When they're sleeping.
Dr. Mason: When they're sleeping instead of using, you know, an indwelling rectal probe. But that's kind of a hard sell to get people to wear that for, like, I don't know, 10 weeks. I don't think they're going to go for it. We're going to measure depression symptoms daily using smartphones so that we can actually see when symptoms are changing. We're going to measure all those biomarkers, and we're going to have all these in relation to each other. And one of the things I really hope we discover, too, is, how willing are people to do this kind of sauna treatment? And then, you know, obviously, seeing how long it lasts. We're going to measure outcomes further than one week and six weeks, obviously. But what my hope is, is that we might be able to develop almost a booster method if, in the future, this seems like a good idea after this next study. And I really hope it does. But you see on the internet that you can buy all these sauna tents that you can use at home. You know, with people...there's always a picture.
Dr. Patrick: Oh, people have them, yeah.
Dr. Mason: And they've got their hands out, and they're reading their magazine, and their head is out, and it looks kind of funny. You could see them on all the different websites. Well, what if we actually need to do a certain number of this intensity of whole-body heating, like the kind that we're talking about here? But then at home, it can be supplemented, and it could be maintained or sustained in this way. And that's a great model moving forward. Would people rather, you know, take drugs that maybe aren't working so well, or maybe come with a certain number of side effects, or say, "Oh, once a week, I have to sit in this thing for 45 minutes and read a magazine," right? So if we can develop a longer-term model for maintaining wellness and maintaining reductions in depression symptoms, that would be a huge win.
Dr. Patrick: Well, you are really moving this field forward. I know that Chuck's sort of moved on to other types of research. And so, you know, these studies are, in my opinion, opening the door for many other potential research studies. People could start to look at Finnish sauna, they could start to look at stuff that people..."Well maybe we can just, you know, find an effect by going for 20 minutes at 175 degrees Fahrenheit." You know, there's all sorts of research that is opened up, you know, where people just don't even know to study this. The hope is that...
Dr. Mason: There's so many open questions.
Dr. Patrick: ...more people will study it, you know, because...and then, can this be applied to like, a hot bath, or a Jacuzzi or...you know. Because there are, as you know, like, small clinical studies showing hot baths can improve with depressive symptoms and people with depressive disorder.
Dr. Mason: So there was a 2017 paper with hot baths, and they did see that, two weeks out, that they had improved those symptoms, but the reduction had faded some by four weeks. But, of note, again, that says something about the temperature. Those people got into that tub at that hot temperature, they weren't warmed up to it, and it was a pretty short hot tub. I think it was like 23 minutes or so. So yes, there are these small studies, and taken together, we're starting to be able to see these patterns of what might matter. Being in there longer, getting to a certain temperature, staying at that temperature, you know, these things. But there are so many research questions that we need to answer in this field, but it's just positively overwhelming. But I'm so excited about the next pair of trials that we're going to be doing. And I'm so glad that you're on board to be doing all of this biomarker assessment with us, and it's going to be a blast.
Dr. Patrick: The fact that it's happening is almost kind of, like, hard to believe. I'm like, "Wow, this is actually happening soon." So I can't wait for it to start. But...
Dr. Mason: You and me both.
Dr. Patrick: Let's move on to another area of...really big area of your expertise. And that is helping treat people with chronic insomnia and using non-pharmacologic treatments for chronic insomnia. Maybe we could start with...I mean, so many people have sleepless nights. There's a lot of people that perhaps they drink too much coffee later in the day, or they have a life event that keeps them stressed and psychologically aroused or they're having too much bright blue light exposure inhibiting their melatonin at night, so they're sort of becoming these night owls from, like, an environmental, you know, stimulus perspective. What's the difference...like, chronic insomnia, like, people that actually have insomnia versus someone who has a chronotype, someone who has a genetic predisposition to being like a night owl, where they stay up really late and then, like, sleep, like, most of the day? Like, there are people that just genetically are predisposed to that. Can you talk about...?
Dr. Mason: Yeah, absolutely. So I know you covered a ton in your podcast with Dr. Satchin Panda about circadian stuff. And that is huge. And there's all kinds of ways that you can mess up your sleep with light, and caffeine, and all those things. Chronotypes, whether you're an evening person or a morning person, those exist. And I think the data are that, you know, some...it's roughly a third, a third, a third. A third-ish of people are morning people, a third-ish of people are evening people, and then a third-ish are somewhere in the middle. And what does that mean? For a lot of people, that just means they feel like they think best, they're their most creative, and they feel best at that time of day. It's pretty biologically determined. Now, of course, we can perturb it with lights and crazy things, but it is pretty biologically determined. And the way that our society is built, it's to favor the larks, the morning people, not the night owls, right? Because we've got work, kids, school, all kinds of stuff starts super early in the morning. And that's hurting the evening people in two ways. One, it's forcing them to get up early. So they're missing out on sleep because they're already going to bed late. And, two, they're not performing well because the morning is not their time to shine. They don't perform that great then. They perform best in the evening. So society isn't set up so well for these evening people. It's really biased toward the morning people. And a chronotype isn't necessarily a sleep problem. It poses more health risks for night owls. But insomnia is something different altogether. Many people will experience insomnia over the course of their lifetime. A lot of people think, "Well, wait, isn't it super genetic?" Well, there's some genetics to it, like 20 to 45-ish percent of insomnia is genetic. But that means that a lot of it is not. A lot of it is due to our own experience, our own behavior. And insomnia is really difficulty falling asleep, difficulty staying asleep, or difficulty with waking up too early in the morning and not being able to get out of bed. For this to be happening at least three nights or so a week, for it to have bee going on for at least three months, and for it to be distressing. That's key, it has to be distressing. So chronotypes and insomnia are pretty different. And every now and then, I get someone referred to me who says, "Oh, you know, I'm an evening person, and I want to become a morning person in two months, please. Like, that's my goal." And I say, "Oh, dear. I don't think that we can change that." And we can talk about ways to work with it. But changing a chronotype is not really something you can just do. That's pretty biologically, genetically determined. But if someone is referred to me as saying, "I can't fall asleep. This started like eight years ago when I changed my job, and I got really stressed out because now I have to perform every Tuesday at some sort of big meeting," or something like this.
Dr. Patrick: What are the main causes of insomnia? Is it stress? Is there triggers?
Dr. Mason: Yeah. So there's a lot of different things that can cause insomnia. A big one is change. It's pretty funny, when patients come to me, I always do...I get halfway through an interview asking about a bunch of different things about their sleep. And then in the middle of my interview, I say, "When did this start? What caused this?" And by asking those other questions first, I get all these other, like, useful details. But you'll often hear "Well, you know, I retired. I used to work 9 to 5, and then I retired. And I was all set up to play golf, go to brunch, read books, do all these things, but then I couldn't sleep." Because it was a huge change to their schedule. They didn't have those zeitgebers anymore during the day, things that anchor them to their 24-hour clock. They didn't have a time they had to get up. They stopped using an alarm. They didn't have to be somewhere at a certain time, so that can be a major change. Other major changes that can lead to insomnia are changes in relationship status, a breakup, losing a job, having a kid, raising a kid. There's a lot of different things that can cause insomnia. However, things that maintain insomnia are generally not the same things as what cause insomnia. For example, let's say someone loses their job. It's really stressful, they get fired unexpectedly, didn't see it coming, really upsetting, right? And so they can't sleep, because they're worrying about all kinds of things, "Where is my next paycheck is going to come from? How am I going to do all these things?" And they start, you know, reading in bed, and listening to music in bed, and trying to do calming things when they're not sleeping, because they're like, "Oh, I can't sleep. I might as well read." Or, "Oh, I might as well watch that show. I guess I could just bring my computer in here."
Dr. Patrick: Facebook.
Dr. Mason: Yeah, "I guess I could get into it. I guess I could bring my computer in bed and just start working on some emails, applying for some more jobs." And then all of a sudden, they're doing all these things in bed. Fast forward three months, they've got a new job, but you know what, they're still taking their computer into bed, checking Twitter in bed, doing all these things, and then wondering why, when they put the things away to go to bed, they can't get to sleep. Well, now, it's these bad sleep hygiene behaviors that are perpetuating their insomnia, not the fact that they lost a job three months ago. That's over with. They got a new job now. So the things that are perpetuating it are the behaviors they actually used to try and help themselves earlier on. [crosstalk 00:53:47.521].
Dr. Patrick: Which then become bad behaviors. - Dr. Mason]: Huh?
Dr. Patrick: Do they become bad behaviors? Would you call them bad behavior? Bad sleep behaviors.
Dr. Mason: Oh, I would say it becomes bad sleep behavior. It's like...
Dr. Patrick: Okay, so you do something... Okay yeah, go ahead.
Dr. Mason: I was going to say, things like napping, things like...and I can talk a little bit about napping, because it's a double-edged sword. But things like napping, things like trying to sleep in on the weekends, using sleep pills, like over-the-counter sleep aids to try and get to sleep, using things that aren't over-the-counter to try to get to sleep. Canceling activities, canceling workouts, skipping them because you're just too tired. So starting to do all of these handicapping activities that are actually detracting from what you really want to be doing, which is building up adenosine during the day. And I know that you or Dr. Matthew Walker talked about how caffeine impacts sleep, and how you really want to accrue sleep drive during the day so that you can fall asleep at night. Well, guess what, if you're taking long naps during the day, you're decreasing the sleep drive that you have at the end of the day that helps capitulate you and asleep and keep you asleep. And if you never used to take naps because you used to sleep fine because you didn't used to do all these other things, it's kind of this feed forward process. And like you've talked about on many podcasts, caffeine. I don't have a problem with caffeine, but if you're drinking it later in the day, it's still very much active when you're trying to go to sleep. It messes with all kinds of things. Similarly, you might develop patterns of using your bright, bright computer screen very, very late at night, when you didn't used to do that before you had a major stressor that happened. So all of these different kinds of behaviors can perpetuate sleep problems. And in the treatment that I do, cognitive behavioral therapy for insomnia, we focus on a bunch of things. We focus on sleep hygiene, and something called stimulus control. We focus on something called sleep restriction, which is not sleep deprivation. I'll mention that in a minute. Cognitive techniques, and then relaxation techniques. So the sleep hygiene I just went over. Stimulus control is going back to basics with the bed. Nothing in bed except for sleep or sex, that's it. No listening to podcasts, no watching TV, no fighting with your spouse, no wondering where your kid is going to apply to college. None of that stuff...
Dr. Patrick: No iPads, social media.
Dr. Mason: None of it in bed, stimulus control. The only thing we do in bed...
Dr. Patrick: No phones in bed.
Dr. Mason: No, oh my gosh. I've got stories about phones. No phones in bed, just sleep or sex. And that means that if you can't sleep, and you're in your bed, and you're laying there worrying, you are violating the rule. You have to get out of bed, and you have to go to the couch or go somewhere else and finish you're worrying or finish whatever you're doing, and then you can go back to bed. And a lot of people don't like that. They think it sounds so hard and awful. But by the time someone's in my office seeing me for sleep problems, I basically say "Look, treatment with me is five weeks of your life. How long have you been struggling with this sleep problem? Worth it? I know you've been on my waitlist for at least 6, 12 months. So if you've been waiting this long to do this, give it a college try, really do it. How much worse can it get?" And there's a really great book that can guide people, by the way, through this whole treatment on their own, if you want, and I can give you the link for that.
Dr. Patrick: What's the book called?
Dr. Mason: It's called "Quiet Your Mind and Get to Sleep."
Dr. Patrick: Okay, that's the one I just ordered because you mentioned it.
Dr. Mason: Yeah, It's great.
Dr. Patrick: I got two copies, so I'm giving one to my mom because...
Dr. Mason: Outstanding.
Dr. Patrick: ...she needs it.
Dr. Mason: Dr. Rachel Manber at Stanford wrote that book, and the foreword was written by Dr. Richard Bootzin, who was the professor from whom I learned this treatment at the University of Arizona. So we've gotten through to...we talked about sleep hygiene, stimulus control, sleep restriction. What that means is we take the amount of time that someone is in bed every night, and we focus on that. Instead of just being in bed doing things, what I do to figure out how long someone should actually be in bed is, the first week that they are with me, they're given a wake time. They have to wake up at that same time every single day for seven days. I always joke with them, "Any day ending in D-A-Y, you have to get up at that time. Include Saturday and Sunday," right? And Dr. Panda spoke all about how important it is to not wake up at different times and how that's like giving yourself artificial jetlag, and all that stuff. So I have patients do that for seven days. But they go to bed whenever they're tired, whenever they're actually sleepy. And we calculate how much time each night, on average, are they sleeping. And over the course of that week, we get an average per night amount of time that they're sleeping. Let's say that turns out that, on average, you sleep seven hours a night, and that your wake time is 8 a.m. That would mean that in order to figure out what your bedtime should be, I work backwards from 8 a.m. I go from 8 a.m. to 1 a.m. And then I add 30 minutes of grace, because that's what we do. And so then I would say, "Rhonda, your bedtime is the bedtime of your childhood dreams. Your bedtime is 12:30 at night. You get to stay up all the way till 12:30, and guess what, not only do you get to stay up that late, you can't go to bed before then. You have to go to bed at that time or after once you're sleepy." And what this actually does is this restricts the amount of time that people are in their beds, the amount of time that they can actually sleep. And pretty quickly, patients will start to get pretty darn good quality sleep during that seven and a half hours. For the first few weeks, it's a struggle bus. They're getting out of bed when they can't sleep, getting back in bed, etc. But, eventually, they're getting pretty deep sleep during that time, pretty good sleep because they're building up so much sleep pressure during the day. And then, during treatment, we extend it back by 15 minutes a week as they demonstrate that they can keep their efficiency, at least 85%. What is efficiency? The amount of time that you're sleeping divided by the total amount of time that you're in bed. And we have patients keep detailed sleep logs about that. There's an example log in that book that you just ordered. So we do that sleep restriction. Then we do the cognitive techniques where we work with people's worries, and thoughts, and how those serve them, and how they don't. And how reflective of reality they are and how much they need to be changed.
Dr. Patrick: Thinking about that negative Twitter comment or, you know, stress at work, you got deadlines, or, yeah, all those things.
Dr. Mason: All that kind of stuff.
Dr. Patrick: Where you're going to send your child to preschool.
Dr. Mason: Big one, big one. I've had patients come in, and their presenting problem has been, "My daughter's majoring in English." I'm like, "Okay." So you get every kind of reason for people saying that they have sleep problems.
Dr. Patrick: Okay, so what do you do? I mean, how do you...that's hard to...
Dr. Mason: It is.
Dr. Patrick: ...deal with, isn't it?
Dr. Mason: Yeah, yeah, there's a bunch of...
Dr. Patrick: When I lay down, I mean, that's one of my problems is, like, that'll become active. It hasn't been active all day, but when I lay down at night, it's...
Dr. Mason: You know, whatever we don't have time to deal with during the day, or whatever we choose not to deal with during the day, it's going to make an appearance at night. It's going to come in and swoop and say, "Hello, here I am, like, you get to deal with me now when you want to be sleeping." So there's a number of different types of tools that we use to work with thoughts and feelings. Have you ever heard the thought, "Don't believe everything you think?"
Dr. Patrick: Yes.
Dr. Mason: "It can be pretty dangerous." Right. So that comes to mind. Working with thoughts...an initial way to think about these approaches is that we identify what we call dysfunctional thoughts. So the thoughts that, you know, they're not really serving us, and, also, they're not super true. So, for example, black and white thinking, right? "If I don't nail this interview, my career is over," right? Like, these complete black and whites. We've also got personalization-type things, "Oh, that person left a negative comment in my Twitter. That must mean I am the worst presenter ever," right? So we can take these things. And then there's also my favorite...one of my fan favorites is "shoulding" all over people, or "shoulding" all over yourself. "I should be doing this. I should be doing that. I should have that done," right? So these kinds of thoughts. Whenever a thought falls into a particular category of dysfunctional thought...and I have a fun list that I can share with you of different types of these, chances are the thought is not all the way true. And we do an exercise called the "thought record" where we look at evidence for thought, evidence that it's true. We look at evidence that it isn't true. And I mean, we really look. I have spent an hour at a time on one thought with a patient before, where we look for all of the possible evidence that it's true, all of the possible evidence that it's not true. And then we have to develop a new thought that acknowledges both the evidence that it is true and the evidence that it isn't true.
Dr. Patrick: Can you give an example?
Dr. Mason: I sure can. Let's pick a flavor. Let's say that you are having the thought, "If I don't get a perfect night of sleep tonight, I am going to just bomb my presentation tomorrow." That's a horrible thing to be thinking about right when you're trying to go to sleep, right? "Oh, I really need to sleep right now because I'm going to be terrible on this presentation tomorrow." Well, what is the evidence that it's true? Well, maybe this person has before not done great the night after a night of sleep. "Oh, I've performed less bad after a night of sleep." Or, I'm sorry, "I've performed..."
Dr. Patrick: Sleep deprivation, yeah.
Dr. Mason: Yeah. "I've performed not as well as I usually do after a bad night of sleep." Or, you know, "I've gotten feedback that my talk wasn't so great after a bad night of sleep before." But then let's look at it isn't true. "There have been plenty of times I have performed on a poor night of sleep. There was that time that I slept overnight at an airport on the way to a conference, and I still pulled off the talk, and it was fine," right? So we have to look at evidence that it's not necessarily true. Also, I can't predict the future. I don't know if I'm going to sleep well tonight or not, right? I haven't decided. I don't know. And then what we do is we developed an adaptive thought, which is, "Well, although I haven't always performed my best on poor nights of sleep, there are plenty of times that I've done just well, giving a talk after a poor night of sleep." And the key thing with this is that, is that adaptive thought just Pollyanna? No. But it's much more reflective of reality than, "If I don't get eight hours of sleep, I'm going to bomb this presentation," right? So we develop a thought that is much more reflective of reality, and then we evaluate how we feel. So, for example, when you have the thought, "I am going to bomb this presentation tomorrow if I don't get eight hours of sleep." How anxious do you feel on a scale from 1 to 10? Let's say it's like a nine, pretty high.
Dr. Patrick: Yeah, depends on the presentation, yeah.
Dr. Mason: Right, sure. But then if we have this other thought, if we adopt a new thought that says, "I don't always perform my best after a poor night of sleep, but I've done it a bunch, and it's gone fine." When we have that thought, our anxiety level on a 1 to 10 isn't like a 9. It might still be like a 5, or maybe a 6, but it's not as high. So we're learning how to match the appropriate amount of the emotion to the thought that is more reflective of reality.
Dr. Patrick: You've listed a lot of things here. We've got the sleep hygiene, we've got the...
Dr. Mason: Stimulus control.
Dr. Patrick: The stimulus control, right.
Dr. Mason: Sleep restriction.
Dr. Patrick: And then the...
Dr. Mason: Cognitive techniques.
Dr. Patrick: Right. And then there was...
Dr. Mason: And then there's relaxation techniques.
Dr. Patrick: Relaxation, yeah.
Dr. Mason: Things like progressive muscle relaxation. Are you familiar with this one?
Dr. Patrick: No.
Dr. Mason: So progressive muscle relaxation is a practice whereby you focus on different muscles in your body, tensing them, squeezing them, and then letting them go, and squeezing them and then letting them go. And then you're focusing on a different part of your body, and you're tensing it, and you're letting it go. And this way, you're getting out of your head and into your body.
Dr. Patrick: Kind of like the breathing exercises [crosstalk 01:05:02.474].
Dr. Mason: It's a lot like a body scan, except for in a body scan, which is more of a mindfulness practice, you're noticing the part of the body. I'm noticing, are my hands warm or cold? And then I'm moving on to my elbows, are they stiff? Progressive muscle relaxation is more active because you're actually squeezing them. And what's always interesting to people is when they get to their shoulders, and they go squeeze their shoulders, and they realize, "Oh, wait, my shoulders are already squeezed, just let them go." That's another major part of this treatment. What I think you're about to ask is, what are the most important ones?
Dr. Patrick: Yeah, like, are they all equal? Are there some that are more important?
Dr. Mason: No, they're not all created equal. And what we know from studies that have been termed "dismantling studies," where they've taken this whole intervention, and they've taken it apart, and they've seen, well, which pieces are most important for good outcomes, we know that the pieces that are really important are the sleep restriction part, matching the amount of time that you're in bed to the amount of time that you can actually sleep. And also the stimulus control, don't do anything in bed that isn't sleep or sex. I often will ask people, "Do you sleep better when you're traveling for work in hotels or on vacation?" And people say "Well, yes, I'm on vacation." And I'm like, "Well, what about when you're traveling for work?" And they say, "Well, yes, actually, I do sleep better when I'm traveling from work." "Why's that?" "You're not sleeping in your bed." "What do you associate your bed with?" "Sleeplessness, anxiousness, not sleeping, being frustrated that you can't sleep." You get all these associations with your bed that we need to fix in cognitive behavioral therapy for insomnia. So we're reducing bed dread, and stimulus control is very, very responsible for that change.
Dr. Patrick: So this is a very effective non-pharmacological treatment for insomnia. I personally know...I have a family member that has insomnia, and they have gone to pharmacological treatment, very common. Ambien is a very common one.
Dr. Mason: Very common.
Dr. Patrick: How do you get...I mean, is it possible to get...so I can tell you from, you know, listening to the experience of this person, they are convinced they cannot see without Ambien. And, in fact, they've tried to quit Ambien before. They've done this, like, you know, weaning off. And, certainly, they've missed days because, like, maybe their prescription wasn't filled, like, whatever. And missing it was, like, they can't sleep at all. And it's like, "Well, what's going on if you are completely, you know, dependent on this drug to sleep?" Like, that is terrifying. Not to mention the side effects with things like Ambien where you've got... I'll tell you, like, this person, like, they'll wake up in the middle of the night and just start eating, and not remember it. And do weird things like...just weird things that they've done the middle of the night. And also, like, memory-wise, it seems like it's affecting like...like, there's something. And there's a literature there that, you know, there can be an association with dementia. And so how does a person shift from that to cognitive behavioral therapy for insomnia, CBTi?
Dr. Mason: Great question. So whenever a new study comes out in the news about the effects of benzodiazepines on sleep, or Ambien, or Lunesta, or Sonata, or any of these drugs on sleep, I get a new influx of referrals because people think, "I need to get off these drugs now. Never mind that I've been on it for 30 years, I need to get off of it this week." And the example you gave is great. When people try and quit, like, just by quitting, for example, they don't sleep, or if they try and taper it themselves...
Dr. Patrick: And then they don't want to quit.
Dr. Mason: And then they don't want to quit. It's a vicious cycle.
Dr. Patrick: It is.
Dr. Mason: It's really hard. And so what I often will notice about folks who want to quit medications is that they're pretty anxious about it. No one's really very calm about quitting Ambien. It's not just this easy transition, adding a new vitamin, for example. So what I do is I work with providers because, yes, using CBTi, cognitive behavioral therapy for insomnia, as part of your plan for quitting medications is a totally great one. And I'm not a prescriber, I'm not a physician. I'm a clinical psychologist. And so I work with the prescribers, which are generally psychiatrists, sometimes internal medicine doctors, on a taper plan. And you mentioned that your family member has tried a taper plan before. The approach that I've taken over the past many years has been what I would call an extraordinarily extended taper plan. Most of these sleep drugs are pills that you can cut with razor blades. They don't come in very convenient, small sizes. I think the smallest Ambien you can get is 5 milligrams. And so what I have people do is I have them by gem scales on Amazon or whatever. And these scales can measure .0 to like .00 of a gram, like, very, very small amounts. And instead of going from 5 to, let's say, cutting it in half, just to 2.5, we'll go from 5 to 4.9 for a few weeks. And I challenge people to detect the difference between 4.9 and 5 physiologically, but, psychologically, there's something there. People need to get used to this idea that, "Okay, I can fall asleep with less than 5 milligrams of Ambien. I can fall asleep with 4.9 milligrams." Now, some people, I always gauge how anxious they are about the change. If going from 5 to 4 sounds really stressful, we go from 5 to, you know, 4.9, or whatever it is. And using this really, really slow process both reduces the physiologic rebound insomnia that you described, like when the prescription wasn't refilled, and you skipped it for a night. So we avoid that. And then we also avoid the anxiety aspect of reducing too quickly or being anxious about reducing it by reducing very, very, very slowly. And it's not rocket science, but that's what I do with people. It can take six months to get off of drugs. It can take longer. But if you do it in this slow, steady way, you don't get the reactivity with it. And one of the major aspects of cognitive behavioral therapy for insomnia that we get away from is reactive medication use. People try and go to bed, and then if they can't sleep, then they get up and take a sleep medication. In CBTi, what we do is we standardize it. You take the same dose of the same medication every night, period. That way, it's not reactive. You're not, you know, perturbing your circadian rhythm at different points in the cycle throughout the night with medications. And, this way, we're removing some of that anxious questioning of, "Am I going to take drugs? Should I skip it tonight? Should I try and da, da, da tonight?" from the equation.
Dr. Patrick: But CBTi probably helps for, you know, someone who is trying to taper themselves off a pharmacological treatment for sleep insomnia probably helps, because now they're thinking, "I'm getting this other thing, and this other thing works. It's clinically shown to work."
Dr. Mason: Yes. And it's fixing all the things that their sleep medications sometimes aren't.
Dr. Patrick: Right, underlying...
Dr. Mason: Making your wake time consistent...
Dr. Patrick: ...addressing the issues, right.
Dr. Mason: All of the other issues.
Dr. Patrick: Right, that's causing the actual insomnia, because something is causing it, you know, in most cases.
Dr. Mason: Generally, our own behavior that we've actually done to try and help ourselves.
Dr. Patrick: So you mentioned the book again. Can you say the title of the book? What was it?
Dr. Mason: "Quiet Your Mind and Get to Sleep."
Dr. Patrick: Now, is there a thing...like, do people...obviously, like, you said you had a waitlist of like 6 to 12 months people to get treatment.
Dr. Mason: It has been.
Dr. Patrick: Doesn't seem like it's a very easily accessible thing for people, whereas a lot of people have insomnia. So can people do things like read this book, or is there other ways they can do cognitive behavioral therapy for insomnia?
Dr. Mason: Yes, yes. So that book is great. And I should say it's by Rachel Manber and Colleen Carney. And there is a great association and website, and I can give you the link for that, where people can go type in their zip code, and they can find providers who can do this treatment near where they live. And it's a very well-known, good way of actually finding providers who know how to do this treatment.
Dr. Patrick: What's the name of the website?
Dr. Mason: Oh, I'm completely blanking on it right now. But I feel like it's, like, Academy of Behavioral Sleep Medicine or something like this.
Dr. Patrick: So we'll put that in the show notes where people can find that.
Dr. Mason: Yeah so people can find that. And, you know, there are...that book, for a lot of people, they can use that book. They can do it themselves, and they can improve their sleep on their own if their problem isn't super severe. But there are other apps that I'm aware of, I think there's an app called Sleepio, and it's a cognitive behavioral therapy for insomnia app. And I believe that it's...I'm not sure exactly how people can get it now. I think there's some healthcare plans you can get it through your employer. It's kind of a strange way of getting to it. But there are some apps. There's Insomnia Coach, which I think is maybe still free. I think the VA actually put one out that anybody can use. And that's in Google Play and iTunes stores. But finding people who can do this treatment through the website, that website is great. It's, unfortunately, harder to find than it should be, because the American College of Physicians did say that this should be the first-line treatment for insomnia before a medication for sleep problem is prescribed.
Dr. Patrick: But it's not. It's not.
Dr. Mason: But it's not, because it is difficult to get insurance, all kinds of issues.
Dr. Patrick: It also takes time.
Dr. Mason: Time and effort.
Dr. Patrick: Effort.
Dr. Mason: And it's not easy. And I always tell patients that they're not going to like me very much in week two and three. You're going to want to make a dartboard with my face on it and just play with it, because you're not going to like waking up in the middle of the night, getting out of bed, having to follow all these crazy instructions. But I always just tell people, "Give it five weeks," because that's how long the version I do is. "If you don't give it a shot, you're never going to know if it works."
Dr. Patrick: How long does it last? Like, do you have to continue doing it?
Dr. Mason: That's a great question. It lasts for quite a while. There's a great paper that I always show patients who are particularly worried about biology that shows how people's C-reactive, or hsCRP changes during treatment compared...it's like Tai Chi versus a sleep seminar, versus cognitive behavioral therapy for insomnia. Everybody got one of those three. And what they show is 16 months out, the people who got the CBTi had the greatest reductions in their hsCRP and the biggest improvements in their sleep, lasting all the way out to 16 months, and treatment only occurred in the first 2 months. It's kind of like Santa Claus. Once you know Santa isn't real, you can't unknow that. Once you learn the things you learn in CBTi, you can't unknow them. And you know exactly...
Dr. Patrick: So you're just applying them. You're just doing it, yeah.
Dr. Mason: You know exactly how you can make your sleep worse.
Dr. Patrick: So it reduces inflammatory biomarkers like high sensitivity, C-reactive protein, hsCRP. That's interesting.
Dr. Mason: When your sleep improves, all sorts of things improve.
Dr. Patrick: So it's like a downstream effect of...
Dr. Mason: Sure.
Dr. Patrick: Cool.
Dr. Mason: So, yes, it can last quite a while. And some people find that they can build more flexibility in. Some people find, "You know what, I need to be rigid about this, and it's okay because I'm rewarded with better sleep." I once had a patient who, for 52 weeks after finishing treatment with me, he still did his Excel calculator sleep diary every week. And he emailed it to me. And on the 52nd week, he said, "Dr. Mason, this is the 52nd diary entry. I'm going to stop sending you these, but you can trust that anytime you want to see one, you email me, and I will send it to you." Because he had found that by just keeping his sleep diary every morning for two minutes, that was the price he paid for improved daytime function, better sleep at night, and just all-around better quality of life. So, ultimately, some people carry on with it full bore for the rest of their lives. Other people realize, "Okay, I know how I can be flexible with this program, and I can choose. I'm going to drink four glasses of wine on Saturday night. I know my sleep is going to be bad. It's okay, I'm going to a winery." Make an informed decision about it.
Dr. Patrick: Right. Well, I know we're...okay, we still have some time. Let's move on to the last sort of area that you're actively doing research on and that, you know, also involves a non-pharmacological treatment for, you know, this sort of behavior that can...you know, in a way, it's like, it's a negative behavior. It's insomnia or not sleeping, or, you know, having...in this case, it would be overeating. Whether the overeating is due to stress, or cravings, or some other sort of, you know, reason, as I think we'll get into more on a reward-based sort of, you know, behavior. Let's talk a little bit about some of that, because it is...I have people in my family...I'm sure everyone either is a person that's experienced this or knows someone that is, like, eating junk food or drinking sugar-sweetened beverages. And it's like, "Stop. It's bad for you. I mean, can't you just stop doing it?" I mean, we know..."You know, you're going to give yourself diabetes, you're going to, you know, potentially, like, lose a limb, or have to be on dialysis, or you're going to get cancer. Or I mean, can you just stop doing it? Just stop drinking Coke." You know, why can't people just stop? Why? Why is it so difficult? Because it is. I mean, I've gone through every possible, you know, science explanation in great detail on how terrible it is drinking soda, and it doesn't matter. Because it gets rid of their migraine, makes them feel better. And there's nothing...you know, or it just makes them feel better. I mean, they have to have it. It's like, I just don't understand. So help me understand, because it's incredibly frustrating. I'm the kind of person, I've got a really good...I'm pretty disciplined, and, you know, like, I can stop things. I can pick it up and, like, keep going. And so, like, I just don't understand, why can't people stop doing that? Like, sometimes I'm like, you know, like, what else do you need?
Dr. Mason: Ironclad resolve you have. Well, there's a few really important things to unpack there. First of which is, does someone want to change or not? If someone wants to change, says, "I really want to lose 40 pounds, and I want to stop drinking Coke for my migraines every day. I really want to stop..." That's different than someone saying, "No, I don't want to stop that. I like my Coke for my migraines. I'm not stopping that." Those are very different things, but they're both very challenging. So let's talk about the first one.
Dr. Patrick: Yes, yeah. Because, I mean, a lot of people know drinking Cokes, like, do they want to get, you know, type II diabetes? Do people want that? I guess. So they know that this, like, could, like, really drastically, you know, change the quality of their life.
Dr. Mason: But a big scary thing 20 years away is different...
Dr. Patrick: Right, it's not relevant.
Dr. Mason: ...than a really comforting thing two minutes away.
Dr. Patrick: All right, so let's talk about the person that knows it's bad, would prefer not to be doing the bad behavior, but still just can't stop. Let's talk about that person.
Dr. Mason: Okay, let's start with how that kind of came to be in the first place, right? And I'm going to try and bring the example a little bit further on the pendulum closer to where you might have been one day or at least know someone very closely, who has been. Let's say you're an academic, and you submit a paper that you are just so excited about to get reviewed in a journal. And it gets rejected. And you're feeling terrible. And you walk by the office kitchen...pre-COVID time, you walk by the office kitchen, and you see some doughnuts on the table. And you think, "I'm going to have a doughnut. It sounds really good right now. I'm going to see." And you have the doughnut, and it's rewarding. And in that moment where you were just so down from the rejection of the paper, then you're so up eating this delicious, sugary, rewarding doughnut. Then you're actually going to learn, "Oh, all right, I'm going to remember this. I'm going to remember that when I felt bad, I ate a doughnut and I felt better." And then the next time something bad happens, you do it again. But the point that you're making is that, yeah, although that person is feeling better in that moment, their physiology is not feeling better in the long term. But in that moment, the doughnut is actually serving as negative reinforcement, is removing a noxious stimuli. It's removing all of the negative experience that I'm having from that rejection. It's taking away that rejection for that moment, and I'm just enjoying that doughnut. And so by doing this, by learning this, I'm learning that I can actually apply this in all kinds of areas of my life. "Oh, when bad things happen, I eat a doughnut. I feel better." It gets reinforced. But over time, I realize, "Oh, my jeans don't fit anymore. And, also, I don't feel so great." And all of these other things. And I'm realizing, "Oh, no, like, this is how I feel better. I need to change this, but I don't have another solution." You might try eating celery instead. How does that work? If that worked, we wouldn't be sitting here talking about this. Substituting doesn't work. Or, "Oh, I'm just going to avoid ever seeing a doughnut again for the rest of my life." That's also very precarious. I don't think it's super realistic. You could probably do a lot of avoiding, but still, then are you going to avoid muffins? Other things might serve quite a similar purpose, right? So avoiding, substituting, these are difficult. So, instead, there are a few different...well, there's a few different ways we can go this conversation. I'll go one direction first. One thing that we know can work, and this is outside of the reinforcement thing is...well, actually, I'm going to come back to that. I'm going to stick with the reinforcement. So what we might do with someone who comes in and says, "Yeah, I've got this problem with these doughnuts. I'm eating these doughnuts every time something gets bad." What I might say to them is not just, "Stop it," because that doesn't work. If we just tell people, "Stop it," no, doesn't work. I might say, "Okay, doughnut-eating, it sounds like it's a pretty important strategy." They say, "Yeah, it's super important. It solves, like, all of my feelings of rejection all day. Like, it helps me deal with all of them." Say, "Okay, well, next time, I want you to sit down with that doughnut, and really pay attention." And that person might next time then sit down with that doughnut and realize, "This doughnut isn't very good. It's been sitting in the kitchen all day. It's a little bit stale. This actually isn't very delicious." And might kind of realize, "Oh, you know what? The real reward here is not actually very rewarding." And then, as a result, they might get disenchanted with this behavior. Like, "Oh, I actually don't enjoy this so much." And another example I'll pull for you is actually from quite a while when I was treating patients in a smoking cessation clinic, because everybody knows that smoking isn't good for you, right? And yet, many, many, many, many people do it. So I once had a patient come in, and he said, "You know what, I love smoking. I love it." And he smoked many, many, many cigarettes a day. A couple packs a day of cigarettes. And I said, "Okay, smoking is awesome. I'm going to ask you to smoke." And he was just shocked. I said, "I want you to smoke, and that's part of your homework is smoking." All good. "Part of your homework is actually smoking." So I told him, "I want you to smoke, I want you to really smoke. I want you to sit at the table. In fact, smoking is so important, I don't want you to do anything else, no reading, no coffee, no TV, no, nothing, just smoking." And he said, "All right, no problem." And I told him, "I want you to rate how you feel before and after you smoke. You got to make a whole, like, smoking notebook, because smoking is so important." I mean, he was thrilled, right, because every provider he'd ever gone to had said, "Stop it. Stop it now. Your peripheral neuropathy is going to get worse. Stop." Right? And here I am sitting saying, like, "Smoke. I want you to smoke."
Dr. Patrick: That means stop.
Dr. Mason: Yeah. And so what he actually found was that, you know what, he did love smoking. But he didn't need to smoke two packs a day. He ended up smoking just a handful of cigarettes a day, four or five cigarettes a day, rather than the whole two packs. Because he found that, "Oh when I really just sit and smoke, after a while, I really want to go do something else. I want to go read that paper, drink that coffee, watch that game, do those things." So when he separated it out and got really curious about the process, he did discover that he liked it, and he stuck with it. But for every story like that, there's someone who slows down to smoke and says, "Oh, you know what, this actually tastes terrible. I don't like this."
Dr. Patrick: And this is the mindfulness aspect.
Dr. Mason: This is the mindfulness aspect. And ofttimes, once someone slows down and really sees the reward of what they're doing, "Oh, this actually tastes bad. I don't actually like this," they become disenchanted with it. Because once you know that...
Dr. Patrick: Although vapes don't taste bad these days, right?
Dr. Mason: Huh?
Dr. Patrick: The vapes, there's...
Dr. Mason: Who knows.
Dr. Patrick: Anyway.
Dr. Mason: But that's why I just tell people...that's why I just advocate for really paying attention to what you're doing, and seeing what really clearly is that reward. And what are you really getting from it in that moment. And then, also, we can use other tools to think about the future, which aren't necessarily the mindfulness piece. But just getting really clear about what that reward is can then help us to no longer be so interested in that behavior. We don't have to use willpower to force ourselves to stop, we're actually using our own experience, "Oh, you know what, those doughnuts are stale. I don't actually want that. I only know they're stale because I slowed down long enough to eat it very slowly and carefully and really taste it."
Dr. Patrick: So you're focusing on the reward aspect, right, because you're kind of changing that. So you're talking about the trigger. Your example was the paper that was rejected, but there's so many triggers.
Dr. Mason: So many.
Dr. Patrick: I mean, so many triggers.
Dr. Mason: So many.
Dr. Patrick: And then the behavior, which is eating the doughnuts, and smoking cigarettes, and then they make you feel better, make you feel good. "I feel good. My migraine goes away. I..." you know.
Dr. Mason: Maybe.
Dr. Patrick: But then when you're focusing on it, what is it actually... "Is it making me feel good? Am I..." so you kind of can change that, is that what you're saying? You can change that reward, feeling, or...
Dr. Mason: Yeah, you can see it more clearly what the reward is, and then, all of a sudden, it's not so much so rewarding. And you realize that, actually, there's a different approach that might be more rewarding, which is rather than just eating that doughnut to forget about my rejection, maybe I'd feel better if I just really sat down and worked with my thoughts.
Dr. Patrick: Now, have some of your colleagues...I know that you work with, you know, many people on, you know, doing this, this sort of reward-based eating research. But have they looked at, you know, when people engage in this mindfulness activity for, let's say, if it was the eating or smoking or both, and they're thinking about, "Okay, well, how does this taste? Is it... Oh, it's sweet, like, so sweet. There's nothing in nature that's this sweet." And they're thinking about it. And they're sort of...you're getting more of a negative. Instead of a positive reward, you're getting more of a negative thought, right? In the brain and the reward, does that activation area, like a brain change from the mindfulness during, like, engaging in that mindfulness, like, behavior or thought? Like, can you, like, actually calm down some of the reward pathway?
Dr. Mason: There have been a number of studies with really serious meditators. And I would refer you to some of the work. I know Dr. Judson Brewer has done a bunch of work on looking at actual brain activation in meditators and how, during meditation, their brain pattern activation can actually change. And when we change our perceived reward value of things, for example, yes, we can change those patterns in our brain. And one of the things that... So Jud and I actually did a trial together, where we did a mindful eating intervention for people who said they have way too many cravings that they eat in response to. And the sample was all overweight women. And we gave them this intervention where they had to get curious about their actual behavior. They had to slow down, eat mindfully and really look at what is the true reward of their doing. And we found that people ate in response to their cravings a whole lot less after doing this training. And it wasn't an effortful intervention. It didn't rely on willpower and trying to change. It really focused just on being curious and being open to observing your experience. And that's what's so, so important. When we use different parts of our brain to be anxious or to be fearful, it's more difficult to also be curious and open to experience.
Dr. Mason: So we published a paper. So Dr. Epel and I published a paper a while ago showing that if you ban the sale of sugary beverages, which we did at UCSF all over the campus, and then you also give people a brief motivational intervention where you show them, "Here's how many sugar cubes are in all the Coke you're drinking on a daily basis," and you give them some information that's kind of this brief motivational interviewing-type stuff, these folks will drink less soda over time. Yeah, so it works. Getting rid of it from your environment and then doing brief interventions that actually communicate information, not in a very judgmental way and not in a harsh way and not necessarily in a super scientific way, but just in a visual way, in a way that might be a little bit surprising. Like, "Oh, this many sugar cubes," right? Some things that are different can help people drink less soda. And if people are experiencing immediate rewards with it, I would still encourage them, "Slow down. Slow down gulping that soda. How do you feel after one sip? How do you feel after two sips?" Maybe people will find that, "Oh, you know what, I don't need 16 ounces. I'm really satisfied with 3 ounces, and that's all I need." Maybe you don't have to eat the whole chocolate cake, maybe just actually a few bites. If you really slow down and pay attention to your experience instead of mindlessly eating the chocolate cake while you're watching TV or slurping down that beverage while you're, I don't know, driving, right? So really slowing down and getting curious about how your body feels and what your experience of the thing actually is can help you consume less. In a perfect world, we consume none of the things that are bad for us. But you know what, like you said, we're not going to find a Twinkie in nature, that combination of fat and sugar with no fiber and no protein, right? These are man-made delicacies that are very hard to resist. So I think it's more of a, well, can we learn how to enjoy these things up to the point where they're enjoyable? Like, maybe the first bite is enjoyable, the second bite is good, third bite is good. Maybe the fourth bite, you don't feel so good anymore about it. Oh, it loses a lot of the flavor by the fifth bite. And then maybe we stop, and we're not eating as much of it. It's harm reduction, right?
Dr. Patrick: Do you think this focusing on mindfulness, like when you're engaging in these "bad behaviors" or things that can, you know, lead to negative health outcomes is something that can be broadly applied? So you mentioned two examples, like the eating of, you know, bad foods, or junk foods, or overeating, and the smoking, but, like, there's a lot of different bad...like gambling. Like, is this, you know, reward-based learning and being mindful during the actual behavior and kind of changing the reward a little bit just by being mindful of it? Is that something that [crosstalk 01:35:09.809]?
Dr. Mason: Anything that's an addictive behavior. Opening up Twitter, opening up social media, gambling, you name it.
Dr. Patrick: So how would you apply that to being, like, having an internet addiction type of behavior where you're...
Dr. Mason: Slow down. Get on the internet for two minutes, and then pause. And check in with your body. How do you feel? How, emotionally, do you feel? Is that how you want to feel in that moment? How is reading comments in response to something you posted on the internet making you feel, right? And then really evaluating, "Is this how I want to spend my time? Is this..." So we can use those techniques, but they are hard. Because scrolling on the internet has that rewarding...you know, that dopamine hit all the people who've studied social media and how our brains respond, it's pretty startling. And taking this pause isn't really rewarding. There isn't a natural reward there in pausing and slowing down and noticing that the doughnut is stale, for example, right? So that is challenging. And, you know, I don't know, therefore, that mindfulness is the whole answer to this. I think there's a bunch of other ways we can work with these situations. For example, I do believe in environmental interventions. If there aren't Twinkies in your house at 2 a.m., you can't eat them at 2 a.m., right?
Dr. Patrick: Right, of course.
Dr. Mason: So it's great to just set up your environment such that it's going to promote the healthy choice. And, of course, there's going to be times when you are out to dinner with friends, and you're having drinks, and you're ordering food, and there's loud music, and there's conversation, and there's all these things. And taking a moment to be mindful isn't really in the cards. So it's not going to be all the time. And what we can do environmentally to help ourselves, for example, looking at menus ahead of time, going to restaurants and making decisions, "Okay, I'm going to get this. And I'm going to plan on bringing some home, or I'm going to plan on sharing some." Or making some of these decisions ahead of time when we're not in the moment is a pretty useful tool. There's also some manipulations called episodic future thinking, for example. So if you're sitting here with a plate of cookies in front of you now, how would I feel eating these now? But then also, I'm imagining myself in three weeks at, you know, some event that I wanted to wear a certain dress to or something like this. These exercises where you transport yourself in time to times where you're at future health goals or future other events and then using that to help inform your decision now. These manipulations from Leonard Epstein's lab have shown some effectiveness in changing eating behavior. They've had people listen to recordings of themselves talking about future goals while ordering fast food in, like, food courts in shopping malls, and they've found that it can influence how much they eat. So using some of these kinds of cognitive tools can help us much more than just kind of the stop it approach. There are lots of people though...well, "lots," I don't know if that's the right word. But there's many people like you who can read a paper and say, "This is bad for me. I am not going to do this. And you know what, I'm going to tell my husband to not do it. I'm not going to feed it to my kid. Nobody's doing it," right? And you're able to just do that. But it's different for a lot of people, especially when they've already learned that reward process.
Dr. Patrick: Right, the positive and negative reinforcement and the type of reward learning. I mean, it's very powerful.
Dr. Mason: Very.
Dr. Patrick: And I do kind of like...I've always found it difficult, like, the mindfulness...I'm not going to go into that. But, like, me meditating, it's like, "Oh, I can't do this."
Dr. Mason: It's hard. It's hard.
Dr. Patrick: But I can go for a run and meditate on my run. Or I can go out surfing and sit on my board, and I'm, like, in the moment. But, like, having to sit down and, like, try to meditate, I'm like I just...
Dr. Mason: But that's not what I'm advocating.
Dr. Patrick: It's not. You know, like this curiosity that you mentioned and, like, getting curious about it. Like, "I'm smoking the cigarette. What does it taste like? What does it smell like?" It smells like shit, you know. You know, that's kind of like a different way of approaching this mindfulness, that, you know, I feel like it's a lot more approachable for a lot of people. Okay, well, yeah, I could sit down and think about, you know, how my cigarettes smells, or how, like, this, you know, sweetened beverage tastes, or this sugar doughnut tastes and just focus on that. And when you kind of focus in on those things, you might start to, like, really go, "Wait a minute."
Dr. Mason: Right. And once you notice those things, that the doughnut is stale...
Dr. Patrick: Change the reward, right?
Dr. Mason: Yes, or that, "Oh, actually, this tastes terrible." You can't unknow that, right? And so you become disenchanted with, it's not the default anymore.
Dr. Patrick: Very interesting stuff, Ashley. I'm so happy that we...
Dr. Mason: Me too.
Dr. Patrick: ...had this discussion that. We talked about so many different things. And I know you are on social media. You're on Twitter. Your Twitter handle is Dr. Ashley Mason, @Dr. Ashley Mason. So people can follow you on Twitter. And you also have a website. Is it a lab website?
Dr. Mason: It's the lab website.
Dr. Patrick: Is it the Sea Lab?
Dr. Mason: Yes. S-E-A, so sealab.ucsf.edu.
Dr. Patrick: Sea?
Dr. Mason: S-E-A.
Dr. Patrick: S-E-A.
Dr. Mason: Yeah, sleep, eating, and affect.
Dr. Patrick: Right. Spell it out again. Was it...?
Dr. Mason: [email protected].
Dr. Patrick: Awesome.
Dr. Mason: Or .ucsf.edu. Gosh.
Dr. Patrick: And people can go to the website, find out about what you guys are doing there. And, eventually, you might have a newsletter that people can sign up for to maybe become a future participant in a study of yours or something like that.
Dr. Mason: Sure, yeah, that's where you can learn about the studies that we're doing in the lab, the sleep group treatment, and how to get involved with the lab.
Dr. Patrick: And the study that I'm a small collaborator with you on should be kicking off soon, fingers crossed. And we'll definitely be informing people about that as well. So thank you so much again, Ashley.
Dr. Mason: Thanks for having me. It was a lot of fun.
Dr. Patrick: Totally. Yeah.
Dr. Mason: Okay.
A prescription drug used to treat insomnia (also known as Zolpidem). Ambien is in a class of medications called sedative-hypnotics. It promotes the activity of GABA receptors in the brain, which slows brain activity to allow sleep.
A psychoactive drug prescribed to treat anxiety, insomnia, and seizures. Benzodiazepines, also known as "benzos," activate gamma-aminobutyric acid (GABA) receptors, reducing activity of the central nervous system. Common benzodiazepines include Valium and Xanax.
A highly selective semi-permeable barrier in the brain made up of endothelial cells connected by tight junctions. The blood-brain barrier separates the circulating blood from the brain's extracellular fluid in the central nervous system. Whereas water, lipid-soluble molecules, and some gases can pass through the blood-brain barrier via passive diffusion, molecules such as glucose and amino acids that are crucial to neural function enter via selective transport. The barrier prevents the entry of lipophilic substances that may be neurotoxic via an active transport mechanism.
A type of protein that acts on neurons in the central and peripheral nervous systems. BDNF is a type of neurotrophin – or growth factor – that controls and promotes the growth of new neurons. It is active in the hippocampus, cortex, cerebellum, and basal forebrain – areas involved in learning, long term memory, and executive function. Rodent studies suggest that lactate, one of many so-called exerkines, mediates some of the benefits of exercise on learning and memory via inducing neuronal BDNF expression.[1] Exercise in combination with heat stress increases BDNF more effectively than exercise alone.[2] BDNF is a profoundly universal point of convergence for mechanistically explaining essentially all known activities that promote brain health.
- ^ Helge, Jørn Wulff; Moritz, Thomas; Morville, Thomas; Clemmensen, Christoffer; Dela, Flemming (2020). Plasma Metabolome Profiling Of Resistance Exercise And Endurance Exercise In Humans Cell Reports 33, 13.
- ^ Heyman, Elsa; Goekint, Maaike; Roelands, Bart; Njemini, Rose; Meeusen, Romain (2011). Influence Of Citalopram And Environmental Temperature On Exercise-Induced Changes In BDNF Neuroscience Letters 494, 2.
An individual’s innate tendency to sleep at a particular time during a 24-hour period. Chronotypes, which are based on circadian rhythms, are genetically determined. Disruption of a person’s chronotypic schedule can influence mood, productivity, and disease risk.
CBT focuses on the development of personal coping strategies that target solving current problems and changing unhelpful patterns in cognitions (e.g., thoughts, beliefs, and attitudes), behaviors, and emotional regulation. It was originally designed to treat depression, and is now used for a number of mental health conditions.
A treatment assigned to participants of a clinical trial that is intended to act as a comparator of an experimental condition. Also called a placebo condition.
An infectious disease caused by the novel coronavirus SARS-CoV-2. COVID-19, or coronavirus disease 2019, was first identified in Wuhan, China, in late 2019. The disease manifests primarily as a lower respiratory illness, but it can affect multiple organ systems, including the cardiovascular, neurological, gastrointestinal, and renal systems. Symptoms include fever, cough, fatigue, shortness of breath, and loss of smell and taste. Some infected persons, especially children, are asymptomatic. Severe complications of COVID-19 include pneumonia, sepsis, acute respiratory distress syndrome, kidney failure, multiple organ dysfunction syndrome, and cytokine storm. Treatments currently involve symptom management and supportive care. Mortality varies by country and region, but approximately 6 percent of people living in the United States who are diagnosed with COVID-19 expire.[1] 1
A ring-shaped protein found in blood plasma. CRP levels rise in response to inflammation and infection or following a heart attack, surgery, or trauma. CRP is one of several proteins often referred to as acute phase reactants. Binding to phosphocholine expressed on the surface of dead or dying cells and some bacteria, CRP activates the complement system and promotes phagocytosis by macrophages, resulting in the clearance of apoptotic cells and bacteria. The high-sensitivity CRP test (hsCRP) measures very precise levels in the blood to identify low levels of inflammation associated with the risk of developing cardiovascular disease.
A broad category of small proteins (~5-20 kDa) that are important in cell signaling. Cytokines are short-lived proteins that are released by cells to regulate the function of other cells. Sources of cytokines include macrophages, B lymphocytes, mast cells, endothelial cells, fibroblasts, and various stromal cells. Types of cytokines include chemokines, interferons, interleukins, lymphokines, and tumor necrosis factor.
A mood disorder characterized by profound sadness, fatigue, altered sleep and appetite, as well as feelings of guilt or low self-worth. Depression is often accompanied by perturbations in metabolic, hormonal, and immune function. A critical element in the pathophysiology of depression is inflammation. As a result, elevated biomarkers of inflammation, including the proinflammatory cytokines interleukin-6 and tumor necrosis factor-alpha, are commonly observed in depressed people. Although selective serotonin reuptake inhibitors and cognitive behavioral therapy typically form the first line of treatment for people who have depression, several non-pharmacological adjunct therapies have demonstrated effectiveness in modulating depressive symptoms, including exercise, dietary modification (especially interventions that capitalize on circadian rhythms), meditation, sauna use, and light therapy, among others.
A neurotransmitter best known for its role in motor, motivation, and pleasure control. Dopamine also functions as a paracrine (cell-to-cell) hormone in other parts of the body. It is derived from tyrosine and is the precursor to norepinephrine and epinephrine. Some evidence suggests that dopamine may also be involved in pain modulation.
A term from statistics. Effect size is a number measuring how strongly two variables are related among a population or in a sample of a population being observed in a clinical trial.
An omega-3 fatty acid found in the meat of fatty fish. EPA reduces inflammation in the body and helps counter oxidative stress in cells. It is crucial for modulating behavior and mood and has demonstrated beneficial effects in managing anxiety and depression. EPA may reduce risk of developing certain chronic diseases such as cancer or cardiovascular disease. Dietary sources of EPA include herring, salmon, eel, shrimp and sturgeon.
A treatment for neuropsychiatric disorders in which a brief seizure is induced using mild electric stimulation. ECT is delivered to patients while under anesthesia. ECT can be an effective treatment for major depression when pharmaceutical treatments fail.
The physiological phenomenon of variation in the time interval between heartbeats. It is measured by the variation in the beat-to-beat interval. Decreased parasympathetic nervous system activity or increased sympathetic activity will result in reduced HRV. Reduced HRV has been shown to be a predictor of mortality after myocardial infarction, and a range of other outcomes/conditions may also be associated.[1]
A family of proteins produced by cells in response to exposure to stressful conditions. Heat shock proteins are expressed in response to heat as well as exposure to cold and UV light, and during wound healing and tissue remodeling. Many heat shock proteins function as chaperones by stabilizing new proteins to ensure correct folding or by helping to refold proteins that were damaged by cell stress. A 30-minute 73ºC sauna session in healthy young adults has been shown to cause a robust and sustained increase in the production of heat shock proteins for up to 48 hours afterward.[1]
- ^ Shields, Richard K; Iguchi, Masaki; Littmann, Andrew E.; Chang, Shuo-Hsiu; Wester, Lydia A.; Knipper, Jane S. (2012). Heat Stress And Cardiovascular, Hormonal, And Heat Shock Proteins In Humans Journal Of Athletic Training 47, 2.
An infrared whole-body hyperthermia device manufactured by the German company Heckel. When using a Heckel device, participants undergo continuous monitoring while reclining on an enclosed bed, and the head is kept cool via the application of cooling cloths or packs.
A condition characterized by excessive sweating. Hyperhidrosis is not necessarily related to heat or exercise. It can be treated with prescription antiperspirants, microwave or botox therapy, or pharmaceuticals.
A critical element of the body’s immune response. Inflammation occurs when the body is exposed to harmful stimuli, such as pathogens, damaged cells, or irritants. It is a protective response that involves immune cells, cell-signaling proteins, and pro-inflammatory factors. Acute inflammation occurs after minor injuries or infections and is characterized by local redness, swelling, or fever. Chronic inflammation occurs on the cellular level in response to toxins or other stressors and is often “invisible.” It plays a key role in the development of many chronic diseases, including cancer, cardiovascular disease, and diabetes.
A type of sauna application that uses infrared light to produce radiant heat. Lamps inside the sauna emit infrared light, a type of light with long wavelengths (the opposite of ultraviolet light). Infrared radiation does not cause cellular damage like ultraviolet light; rather, it is absorbed by the skin and heats the whole body.
A sleep disorder characterized by a persistent inability to fall and/or stay asleep. Insomnia is caused by a combination of genetic, physiological, and psychological factors and is often distressful to those who experience it. Common treatments for insomnia include behavioral therapy, identification and treatment of underlying causes, and developing good sleep "hygiene" (habits).
A committee assembled by an institution to review human research. The purpose of an IRB is to oversee human research at universities, hospitals, pharmaceutical companies, and other organizations and ensure participant safety, ethical integrity, and research quality.
Large molecules consisting of a lipid and a polysaccharide with an O-antigen outer core. Lipopolysaccharides are found in the outer membrane of Gram-negative bacteria and elicit strong immune responses in animals through pattern recognition conferred by a toll-like receptor known as TLR4. Even a low dose LPS challenge of 0.6 ng/kg body weight given intravenously can induce a profound, if transient, 25-fold and 100-fold increase in plasma IL-6 and TNF-alpha, respectively.[1] Also known as bacterial endotoxin.
- ^ Boutagy, Nabil E.; McMillan, Ryan P.; Frisard, Madlyn I.; Hulver, Matthew W. (2016). Metabolic Endotoxemia With Obesity: Is It Real And Is It Relevant? Biochimie 124, .
A medication used to treat insomnia. Lunesta is a sedative-hypnotic nonbenzodiazepine medication; however, it works on the same gamma-aminobutyric acid (GABA) receptors that benzodiazepine drugs act on to produce anxiety-relieving and sleep-inducing effects.
A hormone that regulates the sleep-wake cycle in mammals. Melatonin is produced in the pineal gland of the brain and is involved in the expression of more than 500 genes. The greatest influence on melatonin secretion is light: Generally, melatonin levels are low during the day and high during the night. Interestingly, melatonin levels are elevated in blind people, potentially contributing to their decreased cancer risk.[1]
- ^ Feychting M; Osterlund B; Ahlbom A (1998). Reduced cancer incidence among the blind. Epidemiology 9, 5.
The brain's ability to reorganize itself by forming new neural connections throughout life. Neuroplasticity allows the neurons (nerve cells) in the brain to compensate for injury and disease and to adjust their activities in response to new situations or to changes in their environment.
A non-pharmaceutical method of deep muscle relaxation and anxiety relief. When practicing progressive muscle relaxation, a person tenses and then releases their muscles in groups (e.g., feet, legs, abdomen, arms, fingers).
An enclosed space where one bathes in short-term passive exposure to extreme heat. This exposure elicits mild hyperthermia – an increase in the body's core temperature – that induces a thermoregulatory response involving neuroendocrine, cardiovascular, and cytoprotective mechanisms that work together to restore homeostasis and condition the body for future heat stressors. Sauna use is associated with reduced risk of many chronic diseases, including cardiovascular disease, neurodegenerative disorders, and depression, among others.
A treatment or procedure that is intended to mimic an experimental therapy in a clinical trial. Also called placebo therapy. Participants receiving a sham treatment have likely been assigned to the control arm of the trial.
A medication used to treat insomnia. Sonata is a sedative-hypnotic nonbenzodiazepine medication; however, it works on the same gamma-aminobutyric acid (GABA) receptors that benzodiazepine drugs act on to produce anxiety-relieving and sleep-inducing effects.
A class of drugs that are typically used as antidepressants in the treatment of major depressive disorder and anxiety disorders. Some of the drugs that fall under this classification include: Citalopram (Celexa), Escitalopram (Lexapro), Fluoxetine (Prozac), Paroxetine (Paxil, Pexeva), Sertraline (Zoloft).
A term from behavioral psychology. Stimulus control involves the addition or removal of a stimulus or stimuli from a person’s environment to produce a desired behavioral outcome. Stimulus control therapy is commonly used to treat insomnia by reducing the anxiety associated with sleeplessness.
A noncompetitive Chinese martial art. Tai chi, which incorporates gentle movements and postures with mental focus, breathing, and relaxation, is widely practiced for its beneficial effects on mental and physical health. Tai chi may be helpful in treating insomnia.
A homeostatic mechanism by which the body maintains a core temperature in a consistent range. Thermoregulation in humans is controlled by the hypothalamus and may be dysregulated in people who have depression.
A state of elevated core body temperature (38°C to 43°C; 101°F to 109°F). Hyperthermia stresses the body, activating molecular mechanisms that mitigate protein damage and aggregation while promoting endogenous antioxidant, repair, and degradation processes. Whole-body hyperthermia is often used in a clinical setting as a therapeutic strategy to treat various medical conditions, including cancer, fibromyalgia, and depression.
External signals and cues that influence the body's circadian rhythms. Zeitgeber signals elicit alterations in the body's core clock activity, subsequently altering the expression of genes involved in metabolism. Food intake and light are the dominant zeitgeber signals for humans. Zeitgeber is a German portmanteau, meaning "time giver."
Attend Monthly Q&As with Rhonda
Support our work
The FoundMyFitness Q&A happens monthly for premium members. Attend live or listen in our exclusive member-only podcast The Aliquot.
Sauna News
- Hot water immersion more than doubles core body temperature rise compared to traditional saunas, potentially boosting vasodilation, cardiac output, and immune activity.
- Regular infrared sauna use increases blood vessel density in aged muscles by 33%, though muscle size, strength, and protein synthesis remain unchanged.
- Post-exercise hot tubs and saunas show minimal, inconsistent benefits in exercise performance enhancement, despite potential physiological effects.
- Post-exercise infrared sauna use contributes to a 25% increase in jump height and a 6.8% peak power boost in female athletes—a potential tool for enhancing power production.
- More than 3,600 food-contact chemicals used in packaging and storage detected in humans, including several toxic substances associated with cancer, fertility issues, and hormone disruption.