How to improve sleep through exercise-induced acute inflammation and heat induced immune response | Matthew Walker
Get the full length version of this episode as a podcast.
This episode will make a great companion for a long drive.
The BDNF Protocol Guide
An essential checklist for cognitive longevity — filled with specific exercise, heat stress, and omega-3 protocols for boosting BDNF. Enter your email, and we'll deliver it straight to your inbox.
During illness or infection, the body's immune system launches a pro-inflammatory cascade of events that triggers the need for sleep. These events are recapitulated in both exercise and sauna, providing a potential explanation for the sleep-inducing effects of the two activities. In this clip, Dr. Matthew Walker explains how sleep and sauna may induce sleep through their short-term pro-inflammatory effects.
Matt: I think one thing that's I think fascinated me, though, about the benefit of exercise...so exercise also has a really nice, powerful benefit on sleep, although it's a two-way street, and remind me to talk about that, in a good way. But something else has occurred to me with saunas, too. And I was thinking about this, because I think I know that you're a fan. I think you've mentioned this before. One of the ways that you can induce sleep is that you can increase a lot of the immune factors, things like cytokines, you know, things also like TNF-alpha, or...
Rhonda: IL-6.
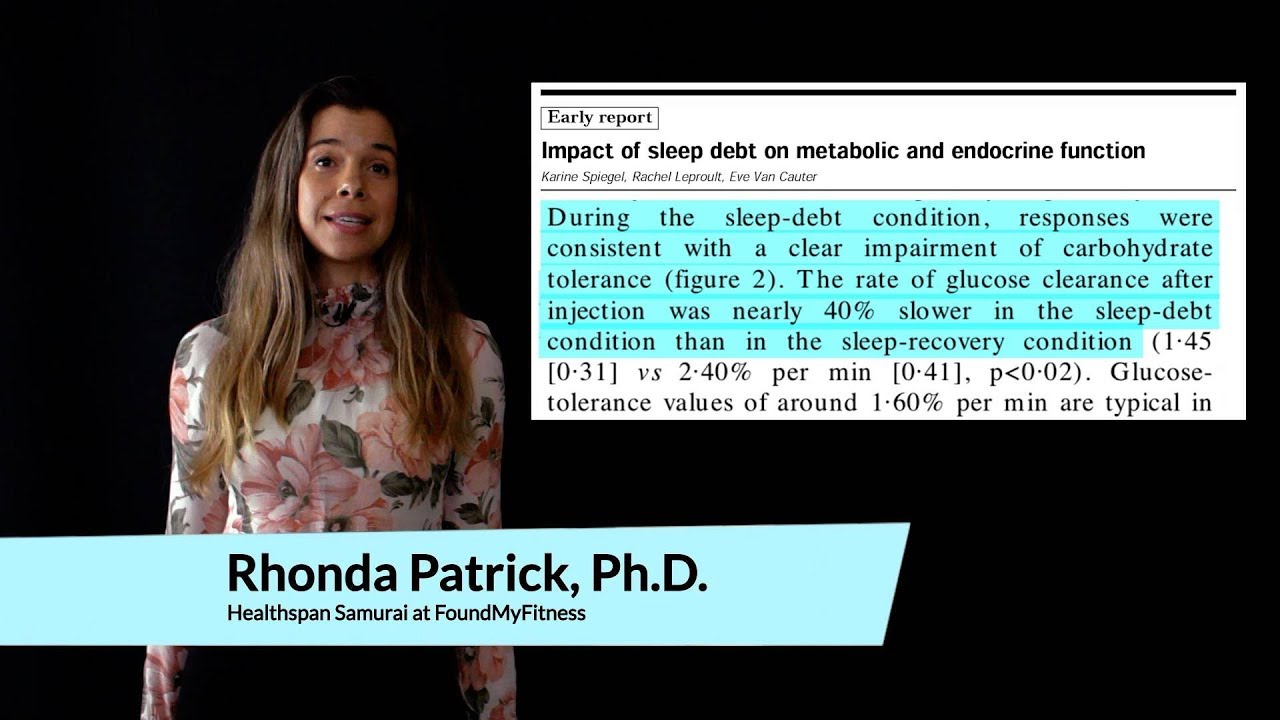
Matt: IL-6. IL-1 even more so, but IL-6 is part of that equation, too. We've known this for some time that if you infect an animal, it will create an immune antibody response, a cytokine cascade. Those cytokines have a direct communication pathway into brain structures, including things like the hypothalamus, which regulates sleep. And it's that immune cascade that is actually a trigger in dialing up the amount of sleep. So when animals get sick, just like when humans get sick, the thing that you want to do is just curl up in bed and go to sleep.
And in fact, you get sleepier as a consequence of being infected. Why is that? The reason is because there is nothing better...Sleep is the Swiss Army knife of health, that no matter what the ailment...
Rhonda: That's so cool. I don't know...
Matt: You know, there is something more than likely in the armament of sleep toolbox, sort of as it were, that will deal with that, and so, and I promise I'm not going off on a tangent here, so the idea is that these immune factors are sleep-instigating.
Rhonda: This is awesome. Wow.
Matt: They are sleep, sort of, you know, they're somnogenic, you know. Somno-sleep, genic-increased genesis, improvement. So what I've been thinking about is whether or not the sauna, the benefit of the sauna, is both thermal, but is also, by way of this powerful immune pathway...
Rhonda: It does.
Matt: ...that you get this.
Rhonda: That's phenomenal.
Matt: And I've read some of the studies, and I'm blanking on his name, you will probably remember his name, they've looked at some of essentially sort of, you know, the sauna-induced immune responses.
Rhonda: Yeah, so that Charles Raison has been doing that work.
Matt: Thank you. Yeah.
Rhonda: Yes.
Matt: Thank you. Brilliant. Yeah, so I've read some of Charles's papers.
Rhonda: Yeah, we had him on the podcast. He was talking about how the sauna induces IL-6 and some of that stuff. And the same thing that happens with exercise. So that's...
Matt: Yes. So that's why I mentioned exercise, which is that I think...
Rhonda: Wow, that's so fascinating.
Matt: So now we're all starting to sort of, you know, realize how the sleep system is augmented, one of those paths, you know, is light. The other is darkness. The other is temperature. But here's a fourth one. The immune system. And we know that you can inject, you know, some of these cytokines into animals, and you can almost induce sleep. It's that powerful.
Rhonda: That's so cool.
Matt: So now I'm starting to think, I wonder if some of the sauna-based benefits and some of the exercise benefits, because when you exercise, you also typically get some of these pro-inflammatory cytokines that sort of get released to perhaps deal with some of, you know, the essential distress. And, you know, I think we've both spoken about this that...
Rhonda: So that way, like if you're exercising a lot, you do seem to require more sleep, or you sleep more?
Matt: Well, we don't know that, but that's my current theory...
Rhonda: Yeah, it's a great hypothesis.
Matt: ...which is that, you know, you possibly...
Rhonda: Are you gonna test that? That's awesome.
Matt: Yeah, we're going to test. So we've just actually been looking at studying not with exercise or with saunas but we've had been looking at sleep and pain. And when you deprive people of sleep, you get a chronic release of these pro-inflammatory cytokines, which is not a good situation. Acute, great, somnogenic, good for the body. But chronic long-term, we're starting to piece together a brain-body-sleep-pain interaction, which I think has, we haven't published this yet, but should have marked implications for the hospital environment. Because the one place where you do not get a good night of sleep, where it's architected against the night of sleep, is the one place where you need sleep the most, and it's usually the one place where you are in pain the most.
And I want a revolution to happen regarding sleep in hospitals. And I'm desperately trying to work with folks. For example, the NHS in the United Kingdom, National Healthcare System there. I would love to work with any hospital system in the U.S. to solve this crisis, I think, of sleep in the hospital environment.
But, to come back to your point, this is a great experiment to do. You know, is exercise-induced acute inflammation, and is sort of, you know, heat/shock sensitive, you know, induction of immune responses by way of saunas or hot baths, are those a pathway triggering good sleep? And if so, can we find novel therapeutics for, you know...
Rhonda: I'll put you in touch with Dr. Jari Laukkanen too. He's in Finland.
Matt: Okay.
Rhonda: He's, like, the leading researcher on saunas and...
Matt: Has he done some of the stuff on longevity?
Rhonda: He's the guy doing all the longevity, Alzheimer's disease, cardiovascular disease...
Matt: Yes, yeah, yeah. I've read some of his work. Yeah, yeah, yeah.
Rhonda: Yeah, I mean, and he's a friend of mine as well. So I'll put you in touch with him.
Matt: Okay.
Rhonda: Because that would be really cool if you guys could...
Matt: If we can start tracking their sleep, you know, and see perhaps. And you can sort of put this into a statistical sort of triangulation, which is called the mediation analysis. And you could see, you know, what's causing that longevity benefit. Because we know for example that the shorter your sleep the shorter your life, that short sleep predicts all-cause mortality. It's also probably one of the most significant lifestyle factors determining whether or not you'll develop Alzheimer's disease. And all of these things I know have been linked to, for example, sauna, which is longevity, decreased susceptibility to the development of dementia and cognitive decline, is part of that...I'm not trying to say it's all about sleep. But, the part of it about sleep, you know...
Rhonda: Really, you know, one of my major interests is aging, increasing healthspan, as well as performance, without the trade-off, and every time I always come back to sleep. The studies, I mean, it just constantly coming back in my face how important sleep is for all those things.
Matt: It's the superordinate lever that transacts all health benefits, you know. It's the tide that rises all of the health boats. And I think it's wonderful that folks, you know, here in Silicon Valley are going after, you know, individual pathways of disease, trying to manipulate, you know, immune pathways or trying to manipulate mTOR for sort of, you know, longevity.
But I think what's been missing in this equation is that there is, you know, an Archimedes lever here. There is one superordinate node, that if you pull that lever, all of the other pathways are instigated, activated. And that superordinate node or lever is this thing called sleep. You know, there is no physiological system that we've been able to measure that isn't wonderfully enhanced by sleep when you get it or demonstrably impaired when you don't get enough.
The death rate from all causes of death for a population in a given time period.
A neurodegenerative disorder characterized by progressive memory loss, spatial disorientation, cognitive dysfunction, and behavioral changes. The pathological hallmarks of Alzheimer's disease include amyloid-beta plaques, tau tangles, and reduced brain glucose uptake. Most cases of Alzheimer's disease do not run in families and are described as "sporadic." The primary risk factor for sporadic Alzheimer's disease is aging, with prevalence roughly doubling every five years after age 65. Roughly one-third of people aged 85 and older have Alzheimer's. The major genetic risk factor for Alzheimer's is a variant in the apolipoprotein E (APOE) gene called APOE4.
A broad category of small proteins (~5-20 kDa) that are important in cell signaling. Cytokines are short-lived proteins that are released by cells to regulate the function of other cells. Sources of cytokines include macrophages, B lymphocytes, mast cells, endothelial cells, fibroblasts, and various stromal cells. Types of cytokines include chemokines, interferons, interleukins, lymphokines, and tumor necrosis factor.
A general term referring to cognitive decline that interferes with normal daily living. Dementia commonly occurs in older age and is characterized by progressive loss of memory, executive function, and reasoning. Approximately 70 percent of all dementia cases are due to Alzheimer’s disease.
Important for the endocrine enhancing properties of exercise. Exerkines are exercise-induced hormonal-like factors which mediate the systemic benefits of exercise through autocrine, paracrine, and/or endocrine properties.[1]
- ^ Helge, Jørn Wulff; Moritz, Thomas; Morville, Thomas; Clemmensen, Christoffer; Dela, Flemming (2020). Plasma Metabolome Profiling Of Resistance Exercise And Endurance Exercise In Humans Cell Reports 33, 13.
The years of a person’s life spent free of disease.
A region of the forebrain below the thalamus that coordinates both the autonomic nervous system and the activity of the pituitary, controlling body temperature, thirst, hunger, and other homeostatic systems, and involved in sleep and emotional activity.
A critical element of the body’s immune response. Inflammation occurs when the body is exposed to harmful stimuli, such as pathogens, damaged cells, or irritants. It is a protective response that involves immune cells, cell-signaling proteins, and pro-inflammatory factors. Acute inflammation occurs after minor injuries or infections and is characterized by local redness, swelling, or fever. Chronic inflammation occurs on the cellular level in response to toxins or other stressors and is often “invisible.” It plays a key role in the development of many chronic diseases, including cancer, cardiovascular disease, and diabetes.
A pro-inflammatory cytokine that plays an important role as a mediator of fever and the acute-phase response. IL-6 is rapidly induced in the context of infection, autoimmunity, or cancer and is produced by almost all stromal and immune cells. Many central homeostatic processes and immunological processes are influenced by IL-6, including the acute-phase response, glucose metabolism, hematopoiesis, regulation of the neuroendocrine system, hyperthermia, fatigue, and loss of appetite. IL-6 also plays a role as an anti-inflammatory cytokine through inhibition of TNF-alpha and IL-1 and activation of IL-1ra and IL-10.
An enzyme that participates in genetic pathways that sense amino acid concentrations and regulate cell growth, cell proliferation, cell motility, cell survival, protein synthesis, autophagy, and transcription. mTOR integrates other pathways including insulin, growth factors (such as IGF-1), and amino acids. It plays key roles in mammalian metabolism and physiology, with important roles in the function of tissues including liver, muscle, white and brown adipose tissue, and the brain. It is dysregulated in many human diseases, such as diabetes, obesity, depression, and certain cancers. mTOR has two subunits, mTORC1 and mTORC2. Also referred to as “mammalian” target of rapamycin.
Rapamycin, the drug for which this pathway is named (and the anti-aging properties of which are the subject of many studies), was discovered in the 1970s and is used as an immunosuppressant in organ donor recipients.
A mixture of solid particles and liquid droplets. It is present in fine inhalable particles, with diameters that are generally 2.5 micrograms or less. Exposure to air pollution promotes oxidative stress and increases the risk of developing many chronic diseases, including cardiovascular disease, cancer, hypertension, and diabetes. Evidence indicates that global air pollution shortens people’s lives on a scale greater than warfare, other forms of violence, parasitic infection, and more.
An antibody that plays key roles in immunity. Secretory IgA is the most abundant antibody in the mucosal immune system, accounting for nearly 20 percent of serum immunoglobulin. It is crucial in protecting the intestinal epithelium from toxins and pathogenic microorganisms.
Sleep-promoting substances or activities. Somnogenic entities include exercise, meditation, and illness, among others.
A proinflammatory cytokine. TNF-alpha is produced by a wide range of cells, including macrophages, lymphocytes, glial cells, and others. TNF-alpha signaling inhibits tumorigenesis, prevents viral replication, and induces fever and apoptosis. Dysregulation of the TNF-alpha signaling pathway has been implicated in a variety of disorders including cancer, autoimmune diseases, Alzheimer’s disease, and depression.
Member only extras:
Learn more about the advantages of a premium membership by clicking below.
Attend Monthly Q&As with Rhonda
Support our work
The FoundMyFitness Q&A happens monthly for premium members. Attend live or listen in our exclusive member-only podcast The Aliquot.
Sleep News
- Regular cannabis use during adolescence may be linked to long-term insomnia risk.
- People with insomnia benefit from regular mind-body or aerobic exercises, with yoga leading as the most effective—increasing total sleep time by nearly two hours.
- The air in children's sleeping areas harbors high chemical pollutant levels, potentially increasing young children's exposure to toxic compounds.
- Resistance training notably improves sleep quality in older adults, outperforming both aerobic and combined exercises.
- Sleep disruption reduces the newly discovered hormone 'raptin,' potentially increasing appetite and promoting weight gain.