Sauna use promotes changes in immune function that may bolster COVID-19 defense
Get the full length version of this episode as a podcast.
This episode will make a great companion for a long drive.
The Omega-3 Supplementation Guide
A blueprint for choosing the right fish oil supplement — filled with specific recommendations, guidelines for interpreting testing data, and dosage protocols.
While no data suggest that sauna use has a direct effect on acute COVID-19 infection, there's a convincing argument that sauna use promotes broader changes in immune function that may bolster defense in a contextually beneficial way. In this way, sauna is probably similar to other healthful activities like exercise rather than the life-saving cures the entire research community is scrambling to identify. Let's support them as a community by taking that search seriously and not confusing the two.
Having said that, robust evidence demonstrates that sauna use promotes mild hyperthermia, which in turn, induces a wide array of beneficial physiological responses. These responses reduce oxidative stress and inflammation and activate cellular defense systems such as heat shock proteins, which provide protection against many diseases.
In fact, data from a 2017 study suggest that sauna use reduces the risk of developing certain chronic or acute respiratory illnesses, including pneumonia, by up to 40 percent.
The sauna’s protective effects on the lungs might be due to reduced oxidative stress and inflammation associated with hyperthermia or direct beneficial effects on lung tissue.
Frequent sauna use may decrease pulmonary congestion and lead to other improvements in lung function including vital capacity, tidal volume, minute ventilation, and forced expiratory volume.
Sauna use also reduced the incidence of common colds in 25 participants who used the sauna one to two times per week for six months compared to 25 controls who did not. It's noteworthy that it took three months before sauna use had a protective effect.
The mechanism by which frequent sauna use reduces the incidence of pneumonia and colds is unknown, but it might be related to modulation of the immune system.
Levels of white blood cells (especially lymphocytes, neutrophils, and basophils) are increased in both trained and non-athletes after sauna use. While these findings are interesting, they are still preliminary and larger studies are needed to confirm.
One of the protective adaptive responses to heat stress is the production of heat shock proteins.
Heat shock proteins (hsps) are a conserved class of proteins with critical roles in maintaining cellular homeostasis and in protecting cells from stressful conditions. Heat shock proteins increased by ~50 percent after 30 minutes in a 163℉ (73℃) sauna in healthy young men and women. Once activated, heat shock proteins can remain so for up to 48 hours.
Heat shock proteins like hsp70 are also readily induced by fever. When hsp70s are released from cells, they can stimulate innate immune responses through toll-like receptors 2 and 4. Increasing evidence suggests that certain heat shock proteins play a role in both innate and adaptive immunity.
Heat shock proteins can directly stimulate innate immune responses, such as the maturation and activation of dendritic cells and the activation of natural killer cells.
This suggests a direct role for heat shock proteins in regulating the innate immune response, which plays an important role in the body's ability to fight off a disease that it has never been exposed to before.
Other modalities of heat stress might promote respiratory health, too.
Unfortunately, most people don't have access to a home sauna, and during these unprecedented times shelter-in-place orders have made it impossible to use public saunas.
However, other modalities of heat stress such as hot baths and exercise have been shown to increase heat shock proteins. One study found that participants that either sat in a hot bath from their waist down for one hour or engaged in 60 minutes of moderate cycling on a stationary bike experienced a ~23 percent increase in hsp70 levels compared to baseline.
Rhonda: The next question has to do with saunas. And the question is, can you discuss whether sauna use may help prevent COVID-19? First of all, there's no data to suggest that using the sauna or other modalities of heat stress such as steam showers or hot baths will have any effect on COVID-19 illness. I can discuss other data that is published on pneumonia and the common cold and also the effect on just the immune system in general. But I can't speak directly to COVID-19 because there is no data to suggest whether or not the sauna will have any effect on COVID-19.
Let's start by discussing lung health. Sauna use has been associated with a reduced risk of developing certain chronic or acute respiratory illnesses, including pneumonia. Sauna use promotes mild hyperthermia, which in turn induces a wide array of physiological responses. These responses reduce oxidative stress and inflammation and activate cellular defense systems that provide protection against many diseases.
So data from a 2017 study suggests that sauna use reduces the risk of developing certain chronic or acute respiratory illnesses, including pneumonia, which is acute respiratory illness characterized by cough, fever, chills, and difficulty breathing. It's a common complication of influenza and other viral illness infections, including COVID-19 as well as bacterial infections. Pneumonia affects people of all ages, but children, older adults, and people who are immunocompromised seem to be most vulnerable. So this study drew on data from a population-based prospective cohort study of more than 2,000 healthy middle-aged men between the age of 42 and 65 years old. And it was conducted in Finland where most people have a home sauna. The average sauna exposure reported in the study was approximately 20 minutes per session and the temperature was 174 degrees Fahrenheit or 79 degrees Celsius. The data was adjusted for a variety of potential confounding factors like body mass index, smoking, status, education level, alcohol consumption, total energy intake, socioeconomic status, physical activity, inflammatory status, and a history of diabetes, heart disease, asthma, bronchitis, or tuberculosis.
So the study revealed that the frequency of sauna use was inversely associated with the incidents of respiratory illness. Men who used the sauna 2 to 3 times weekly were 27% less likely to develop pneumonia than those who used the sauna once a week or not at all. Men who used the sauna 4 to 7 times a week were 41% less likely to develop pneumonia compared to the infrequent sauna users. The sauna's protective effects on the lungs may be due to reduce oxidative stress and inflammation associated with hyperthermia or the direct beneficial effects on lung tissue. Frequent sauna use may decrease pulmonary congestion and lead to other improvements in lung function, including vital capacity, tidal volume, minute ventilation, and forced expiratory volume.
Sauna use has been shown to improve lung function in people with obstructive pulmonary disease. Typical Finnish saunas are not the only type of heat stress that have been shown to be beneficial for lung health. Waon therapy, which uses far-infrared dry saunas also has been shown to improve lung function in patients with chronic pulmonary disease also known as COPD. The temperature of far-infrared saunas are significantly lower than typical Finnish saunas. So they're typically around 140 degrees Fahrenheit. Since the temperature is lower, the duration in many studies is longer, around 45 minutes. And the frequency in many studies is daily for a few weeks. One of the major differences between dry saunas or Finnish saunas and far-infrared saunas is that both dry and Finnish saunas, the heat, the ambient air, and that heat is transferred from the air to the body. But in far-infrared saunas, the thermal radiation is directly used to increase body temperature.
Sauna bathing was shown to reduce the incidents of common cold in 25% participants that use the sauna 1 to 2 times per week for 6 months compared to 25 controls that did not. It took three months before the sauna had a protective effect. The mechanism by which frequent sauna use reduces the incidence of cold is unknown, but it could have to do with the modulation of the immune system. White blood cells, lymphocytes and neutrophil counts were all increased in both trained and non-trained athletes after sauna use. While these findings are interesting, they're still preliminary and larger studies are needed to confirm.
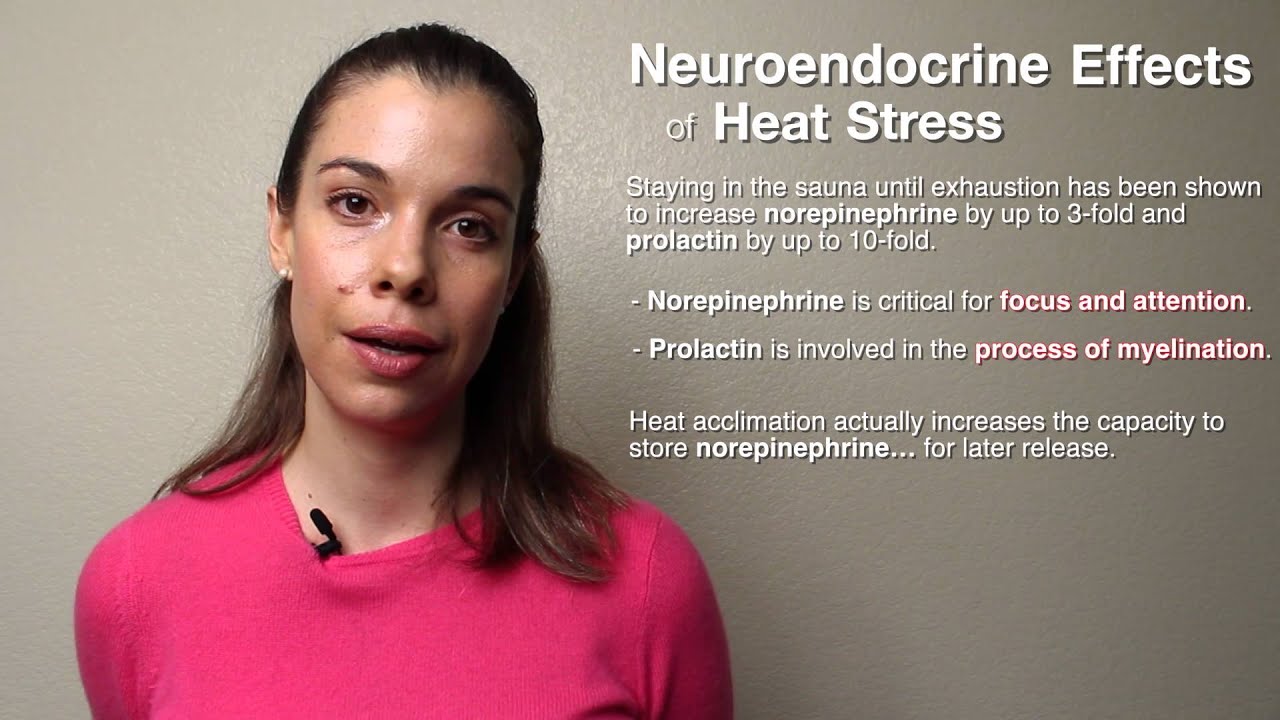
One of the protective adaptive responses to heat stress is the production of heat shock proteins. Heat shocked proteins are a conserved class of proteins with critical roles in maintaining cellular homeostasis and in protecting the cells from stressful conditions. Heat shocked proteins have been shown to be increased by approximately 50% after 30 minutes in 163-degree Fahrenheit sauna in healthy young men and women. Once activated, they can remain so for up to 48 hours. It's been shown that being acclimated to heat, such as from regular sauna use results in the production of more heat shock proteins under normal conditions and even more so under stressful conditions such as cell and tissue injury. This is good because as we age, we make less heat shock protein. So anything to boost them as beneficial.
Heat shocked proteins like heat-shocked protein 70 are also readily induced by fever and when released from cells, heat-shocked protein 70 can stimulate the innate immune response through toll-like receptors 2 and 4. The relationship between exposure temperature and maximal heat shock protein 70 protein levels was linear between normal body temperature of 98.6 degrees Fahrenheit and 105.8 degrees Fahrenheit. So increasing approximately 50% per degree Celsius in human lung epithelial cells. Increasing evidence suggests that certain heat-shocked proteins play a role in both innate and adaptive immunity. Heat shocked proteins can directly stimulate the innate immune responses such as the maturation and activation of dendritic cells and the activation of natural killer cells.
This means that there may be a direct role for heat-shocked proteins in regulating the innate immune response, which plays an important role in the body's ability to fight off a disease that it's never been exposed to before. Heat shock protein 70, when given to mice, acts as an adjuvant and stimulates the innate immune system. It confers protection against, for example, HSV when exposed. In addition to directly impacting the immune function, heat shock proteins such as heat shock protein 70 have also been shown to directly inhibit viral activity and replication of influenza virus A. While the effect of heat shock proteins on viruses is a bit nuanced, the more important thing is that heat shock proteins activate the innate immune system and sauna use has been shown to increase white blood cell and other monocyte levels.
I know many people don't have access to a home sauna and without gyms open, you know, gyms or gyms are closed at this time, so it's kind of impossible for a lot of people to use the sauna. So let's talk a little bit about hot bath since most people do have access to a bathtub. Hot baths have also been shown to increase heat shock proteins, which is good news. One study found that participants that sat in a hot bath from their waist down for one hour were able to increase their heat shock protein levels. So just in summary, it appears as though sauna use is protective against some respiratory illnesses like pneumonia as well as COPD. And it has been shown to be protective against the common cold, it's been shown to increase the innate immune response in terms of increasing white blood cell numbers and other monocyte numbers and it's also known to activate the innate immune response. Hot baths, which also is another modality of heat stress, have been shown to increase heat shock proteins, which are thought to be the main regulator by which...or the main mechanism by which the sauna is modulating the immune system.
A prescription drug used to treat insomnia (also known as Zolpidem). Ambien is in a class of medications called sedative-hypnotics. It promotes the activity of GABA receptors in the brain, which slows brain activity to allow sleep.
A variable that is related to one or more of the other variables in a study. A confounding factor can mask an association that exists between variables or demonstrate an association that does not exist. If confounding factors are not measured and considered, the findings of the study may be biased.
In statistics, a confounder (also confounding variable or confounding factor) is a variable that is correlated (directly or inversely) to both the dependent variable and independent variable.
An infectious disease caused by the novel coronavirus SARS-CoV-2. COVID-19, or coronavirus disease 2019, was first identified in Wuhan, China, in late 2019. The disease manifests primarily as a lower respiratory illness, but it can affect multiple organ systems, including the cardiovascular, neurological, gastrointestinal, and renal systems. Symptoms include fever, cough, fatigue, shortness of breath, and loss of smell and taste. Some infected persons, especially children, are asymptomatic. Severe complications of COVID-19 include pneumonia, sepsis, acute respiratory distress syndrome, kidney failure, multiple organ dysfunction syndrome, and cytokine storm. Treatments currently involve symptom management and supportive care. Mortality varies by country and region, but approximately 6 percent of people living in the United States who are diagnosed with COVID-19 expire.[1] 1
A family of proteins produced by cells in response to exposure to stressful conditions. Heat shock proteins are expressed in response to heat as well as exposure to cold and UV light, and during wound healing and tissue remodeling. Many heat shock proteins function as chaperones by stabilizing new proteins to ensure correct folding or by helping to refold proteins that were damaged by cell stress. A 30-minute 73ºC sauna session in healthy young adults has been shown to cause a robust and sustained increase in the production of heat shock proteins for up to 48 hours afterward.[1]
- ^ Shields, Richard K; Iguchi, Masaki; Littmann, Andrew E.; Chang, Shuo-Hsiu; Wester, Lydia A.; Knipper, Jane S. (2012). Heat Stress And Cardiovascular, Hormonal, And Heat Shock Proteins In Humans Journal Of Athletic Training 47, 2.
An organism’s ability to maintain its internal environment within defined limits that allow it to survive. Homeostasis involves self-regulating processes that return critical bodily systems to a particular “set point” within a narrow range of operation, consistent with the organism’s survival.
A critical element of the body’s immune response. Inflammation occurs when the body is exposed to harmful stimuli, such as pathogens, damaged cells, or irritants. It is a protective response that involves immune cells, cell-signaling proteins, and pro-inflammatory factors. Acute inflammation occurs after minor injuries or infections and is characterized by local redness, swelling, or fever. Chronic inflammation occurs on the cellular level in response to toxins or other stressors and is often “invisible.” It plays a key role in the development of many chronic diseases, including cancer, cardiovascular disease, and diabetes.
A type of white blood cell, also known as a granulocyte. Neutrophils are the most abundant form of blood cell, comprising approximately 60 percent of total cells. They ingest, kill, and digest microbial pathogens, and are the first cells recruited to acute sites of injury. Neutrophils can infiltrate brain structures, driving inflammation and increasing the risk for neurodegenerative disorders, such as Parkinson's disease and Alzheimer's disease.
A result of oxidative metabolism, which causes damage to DNA, lipids, proteins, mitochondria, and the cell. Oxidative stress occurs through the process of oxidative phosphorylation (the generation of energy) in mitochondria. It can also result from the generation of hypochlorite during immune activation.
A prospective cohort study is a type of study, e.g., in sociology or medicine, that follows participants for a particular future time period.
Get email updates with the latest curated healthspan research
Support our work
Every other week premium members receive a special edition newsletter that summarizes all of the latest healthspan research.
Sauna News
- Hot water immersion more than doubles core body temperature rise compared to traditional saunas, potentially boosting vasodilation, cardiac output, and immune activity.
- Regular infrared sauna use increases blood vessel density in aged muscles by 33%, though muscle size, strength, and protein synthesis remain unchanged.
- Post-exercise hot tubs and saunas show minimal, inconsistent benefits in exercise performance enhancement, despite potential physiological effects.
- Post-exercise infrared sauna use contributes to a 25% increase in jump height and a 6.8% peak power boost in female athletes—a potential tool for enhancing power production.
- More than 3,600 food-contact chemicals used in packaging and storage detected in humans, including several toxic substances associated with cancer, fertility issues, and hormone disruption.