How gut microbiome is affected by circadian rhythm and sleep deprivation | Matthew Walker
Get the full length version of this episode as a podcast.
This episode will make a great companion for a long drive.
The BDNF Protocol Guide
An essential checklist for cognitive longevity — filled with specific exercise, heat stress, and omega-3 protocols for boosting BDNF. Enter your email, and we'll deliver it straight to your inbox.
The gut-brain axis, the bidirectional signaling pathway between the gastrointestinal tract and the nervous system, modulates the body's stress response. A key player in this pathway is the gut microbiome, the collection of genomes of the microorganisms that exist in the gastrointestinal tract. Sleep deprivation alters the overall gut microbial make-up, which can promote dysregulation of the microbiome and in turn, altered sleep. In this clip, Dr. Matthew Walker discusses the role that sleep plays in modulating the gut microbiome.
Matt: Now I don't think there's enough evidence right now for me to hang my hat on any dietary prescription for sleep. In five years' time, I think we'll have a very different conversation. I think, you know, absence of evidence is not evidence of absence. I think we'll get there. And I think food is going to be a big part of that equation. I think we have gut microbiome, too. I think that's what we've seen when you, in a few of the studies where you limit people, you sleep deprive them or you put them on a jet lag routine, you see the balance between the sort of bacteriodetes sort of class of the microbiome versus the firmicutes. That ratio goes in a balance that you don't want.
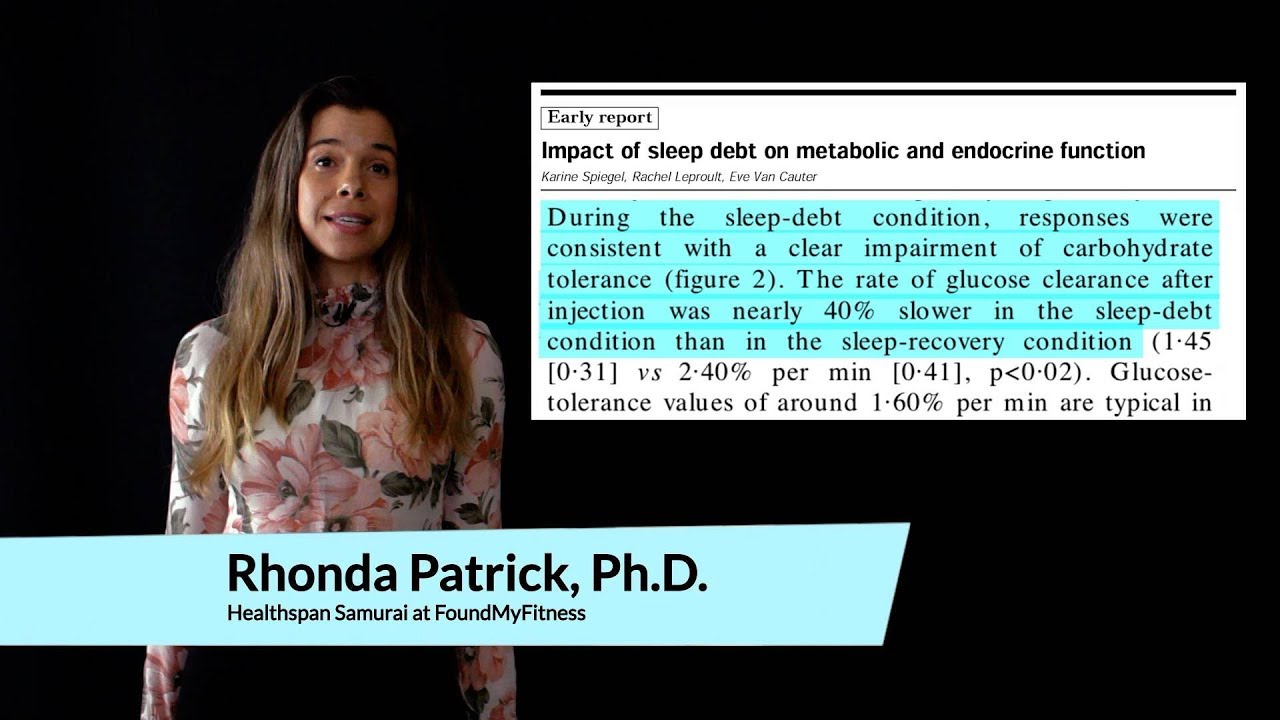
So, typically, in sort of obese people or people with diabetes, you get a higher ratio of the firmicutes relative to the bacteriodetes. When you modulate sleep and you shortchange sleep or you put sleep on a jet lag profile, that's exactly the same gut microbiome sort of dysregulation profile that you see. So I think it's gonna be a great...And I think part of...
Rhonda: Because they're on their own circadian rhythm as well, the...
Matt: They are. Yeah.
Rhonda: So is that why? Because their ratio is changing and then...?
Matt: I think it's possible that it could be a circadian rhythm. I think it's also possible that it could be down to what we described before, which is the fight-or-flight branch of the nervous system, that when you are under slept, it's, like, revving a car but in neutral. It's desperately bad for the engine. That's what happens when you're sleep-deprived. You get this ramping up of your fight-or-flight system, and it just stays there with chronic sleep deprivation for as long as you're chronically sleep-deprived. And one out of every two adults in first world nations is chronically sleep-deprived.
I think it leads to a release of stress chemistry, particularly cortisol. Cortisol is known in the gut microbiome to produce this imbalance. What's the pathway? I think it's probably a bunch of nerve fibers from the brain into the body called the vagus nerve. And we're starting to do a lot of work on this now. I think the vagus nerve we know has a direct mainline pathway or provides a mainline pathway from your brain to your gut. And that's why there is a very powerful brain-gut relationship.
I think that's one of the mechanisms by which the gut is affected by sleep. Which gets me excited, because if that's true, flip the equation, could the gut microbiome be a path through which we can reverse-engineer a signal for better sleep in the brain? I think that now becomes a parsimonious hypothesis, and it's one that I'd like to test as well.
Rhonda: There was a really interesting study looking at the effects of a particular strain. I think it was the rhamnosus strain that...they produce GABA in the gut.
Matt: Yes.
Rhonda: But GABA doesn't cross the blood-brain barrier as far as...I think most evidence suggests it does not.
Matt: No. So the brain has GABA, but it's not coming from the...
Rhonda: Right, right.
Matt: Yeah.
Rhonda: But there was some studies that were speculating that there's, through the vagal nerve, because some of the efferent neurons in the gut were stimulating it, and they were more, like, relaxed or something. They were producing GABA in the brain through the vagal nerve. And GABA affects sleep, right?
Matt: Yeah.
Rhonda: So it sounds like there could definitely be some sort of interesting...
Matt: You know, that's one of...I think the things in anxiety that we see is that it's a failure of the brain to dampen down and basically invoke inhibition throughout the brain to quiet down these regions.
Rhonda: That particular strain of probiotics was shown to help with anxiety. Small trials, clinical trials in humans. Of course, the initial studies were preclinical in animals, but it has been shown to actually help improve...
Matt: It does?
Rhonda: Yeah. [inaudible 02:14:04]...
Matt: My guess is that, if that's true, if you were to look at sleep, I would be surprised not to see a sleep benefit by way of an anxiety reduction. I think, I mean, in my lab, that's probably one of the most reliable things that we see when we deprive people of sleep, of any dose.
Rhonda: That anxiety goes up?
Matt: Anxiety goes up. We've done the dose response curve. We've looked, you know, hour by hour by hour. And as soon as you get past probably about 14 or 15 hours of wakefulness, anxiety starts to increase.
A highly selective semi-permeable barrier in the brain made up of endothelial cells connected by tight junctions. The blood-brain barrier separates the circulating blood from the brain's extracellular fluid in the central nervous system. Whereas water, lipid-soluble molecules, and some gases can pass through the blood-brain barrier via passive diffusion, molecules such as glucose and amino acids that are crucial to neural function enter via selective transport. The barrier prevents the entry of lipophilic substances that may be neurotoxic via an active transport mechanism.
The body’s 24-hour cycles of biological, hormonal, and behavioral patterns. Circadian rhythms modulate a wide array of physiological processes, including the body’s production of hormones that regulate sleep, hunger, metabolism, and others, ultimately influencing body weight, performance, and susceptibility to disease. As much as 80 percent of gene expression in mammals is under circadian control, including genes in the brain, liver, and muscle.[1] Consequently, circadian rhythmicity may have profound implications for human healthspan.
- ^ Dkhissi-Benyahya, Ouria; Chang, Max; Mure, Ludovic S; Benegiamo, Giorgia; Panda, Satchidananda; Le, Hiep D., et al. (2018). Diurnal Transcriptome Atlas Of A Primate Across Major Neural And Peripheral Tissues Science 359, 6381.
A steroid hormone that participates in the body’s stress response. Cortisol is a glucocorticoid hormone produced in humans by the adrenal gland. It is released in response to stress and low blood glucose. Chronic elevated cortisol is associated with accelerated aging. It may damage the hippocampus and impair hippocampus-dependent learning and memory in humans.
The relative ratios of the two major microbial phyla in the human gut. Firmicutes and Bacteroidetes represent 99 percent of the bacteria in the gut. However, the levels of these two dominant bacterial divisions shift in response to a variety of factors, including diet, exercise, physiological and psychological stress, and age, even when taking large inter-individual variation into account. A low Firmicutes to Bacteroidetes ratio is associated with a wide array of diseases, including metabolic dysfunction, cardiovascular disease, obesity, neurological disorders, and autoimmune disease, among others.
A neurotransmitter produced in the brain that blocks impulses between nerve cells. GABA is the major inhibitory neurotransmitter in gray matter.
The collection of genomes of the microorganisms in a given niche. The human microbiome plays key roles in development, immunity, and nutrition. Microbiome dysfunction is associated with the pathology of several conditions, including obesity, depression, and autoimmune disorders such as type 1 diabetes, rheumatoid arthritis, muscular dystrophy, multiple sclerosis, and fibromyalgia.
Member only extras:
Learn more about the advantages of a premium membership by clicking below.
Attend Monthly Q&As with Rhonda
Support our work
The FoundMyFitness Q&A happens monthly for premium members. Attend live or listen in our exclusive member-only podcast The Aliquot.
Sleep News
- Regular cannabis use during adolescence may be linked to long-term insomnia risk.
- People with insomnia benefit from regular mind-body or aerobic exercises, with yoga leading as the most effective—increasing total sleep time by nearly two hours.
- The air in children's sleeping areas harbors high chemical pollutant levels, potentially increasing young children's exposure to toxic compounds.
- Resistance training notably improves sleep quality in older adults, outperforming both aerobic and combined exercises.
- Sleep disruption reduces the newly discovered hormone 'raptin,' potentially increasing appetite and promoting weight gain.