Lack of deep sleep linked with amyloid-beta build up in Alzheimer's disease | Matthew Walker
Get the full length version of this episode as a podcast.
This episode will make a great companion for a long drive.
The Omega-3 Supplementation Guide
A blueprint for choosing the right fish oil supplement — filled with specific recommendations, guidelines for interpreting testing data, and dosage protocols.
During sleep, the brain activates the glymphatic system, a self-cleaning process that rids the brain of metabolic byproducts. One of these byproducts is amyloid-beta, a toxic protein that aggregates and forms plaques in the brain with age and is associated with Alzheimer's disease. Poor sleep promotes the build-up of amyloid-beta, which, in turn, promotes poor sleep, creating a vicious cycle that has direct effects on brain health. In this clip, Dr. Matthew Walker describes the role that sleep plays in modulating the accumulation of amyloid-beta accumulation in the brain.
Rhonda: One that I'm particularly interested in is Alzheimer's disease. It's something that I've been researching for a while. I'm about to get published thankfully soon.
Matt: Congratulations.
Rhonda: Thank you.
Matt: Was this a review paper?
Rhonda: Yeah.
Matt: Oh, please send it to me.
Rhonda: And it happens to do with a gene called APOE4. And I found out that I have one copy of this of this allele. And when I found that out years ago, I was like...it's probably the biggest risk factor for late-onset Alzheimer's disease besides age.
Matt: Yes. So I think one of those alleles, it's about sorts of two to threefold risk.
Rhonda: Two to threefold.
Matt: If you have two of them, it's like an 8 to 12.
Rhonda: Yeah, it's, like, pretty bad. And 25% of the population in the United States has at least one allele. So it's definitely...And just because you have it doesn't mean you're necessarily gonna get Alzheimer's disease.
Matt: That's right.
Rhonda: Not everyone has it. But there's a huge interaction with, you know, diet and lifestyle. Probably the biggest lifestyle interaction with this gene is sleep. And so that was that was where I became very interested in how sleep affects the brain, and how it affects, you know, Alzheimer's disease, and all that. So I'd love to kind of talk a little bit about that.
Matt: Yeah, so we've been doing a lot of this work. We have a large research program here at UC Berkeley at the Sleep Center that is devoted to aging and Alzheimer's disease. And we've been very fortunate to get many grants from the NIH here to study this. I think that the story is fascinating because it's a bi-directional relationship between sleep and the pathology that we know is associated with Alzheimer's disease.
So in Alzheimer's disease, there are at least two protein culprits that we believe are underlying of the brain pathology that seems to create this thing called Alzheimer's. One of them is a sticky toxic protein called beta amyloid that accumulates in these clumps outside of brain cells. And that creates these amyloid plaques that seem to be correlated with your disease risk and disease severity.
The other is a protein that we know probably less about, which is a protein called tau protein. And that sits inside of cells. And it creates a support structure for communicating and funneling many of the critical ingredients up and down your nerve cells to keep them in rude health. And during Alzheimer's disease, that protein starts to sort of fall apart and dismantle. And you get these sort of tau tangles. And the structure of the nerve cell and its ability to transport all of the ingredients that it needs to operate starts to collapse and fails like a tunnel collapsing down.
So one of the discoveries that we made back in 2013 was that I was looking at the distribution of this sticky toxic protein called amyloid in the human brain. And what's fascinating is that it doesn't build up in the brain homogeneously. Amyloid builds up in some parts of the brain far more severely and early in the course of Alzheimer's disease. And other parts actually remain completely uninvaded by this thing called amyloid. In fact, parts of the motor cortex, for example, or parts of the visual cortex, you see almost no amyloid in our Alzheimer's patients. And that's probably the reason why their motor functions and their vision is unchanged.
But one of the earliest places where beta amyloid builds up and then built up most severely in late stages is back, again, in that medial prefrontal cortex that sits right there in between the eyes. Why was I interested in that? I was interested because when we were doing studies where we would map, with all of these electrodes over your head, we would map the deep sleep that you were having.
And we could do some clever mathematical modeling of those deep sleep brain waves. And we could try to triangulate where was the electrical epicenter of those electrical deep brain waves of deep sleep. And it seems as though they come from all over the brain, but the principal epicenter that generates your deep sleep sits right there in the middle part of the prefrontal cortex. It is exactly the same part of the brain that accumulates toxic beta amyloid protein.
Then we've done studies, and other people have done studies before us, that demonstrated, as we age, our sleep gets worse. But not just any type of sleep. Especially that deep quality of sleep that we know and we spoke about is critical for saving and learning and retaining new memories. So all of these jigsaw pieces started to get put together in my head. I thought we need to do some studies. Is it possible that the amount of amyloid that you have in the brain in this sleep-generating center, it should directly predict the deficit in the amount of deep sleep that you get? If it predicts the deficit in the amount of deep sleep, it should predict the deficit in your ability to hold on and retain new memories, which is a hallmark cognitive feature of Alzheimer's disease, difficulty learning, difficulty retaining.
So we did the study, and it's exactly what we found. The more beta amyloid that builds up in this central frontal part of the brain, the less the deep sleep that you have. The less amyloid-related deep sleep that you had, the more forgetful you were the next day rather than the more that you remembered. So this was the first part of the Alzheimer's sleep equation, which is that Alzheimer's disease attacks the deep-sleep-generating regions and you have a diminution of deep sleep, which, in turn, blunts your learning and memory abilities and you become more forgetful.
A far more important discovery was made by an another group, far more important than the one we made, which was essentially the reverse direction, which was to say, "Rather than amyloid sort of decreasing sleep, could sleep actually decrease the amount of amyloid that you get?"
And this is a discovery that was made in rats back in 2009, I believe, was the first evidence that was published in science. A colleague, [inaudible 01:24:09], who is out on the east coast at the University of Rochester, and she made two wonderful discoveries. The first was that we've known for a long time the body has a waste sewage system called the lymphatic system. But the brain doesn't have its own lymphatic system. The lymphatic system does not penetrate the brain. So where does all of the garbage, the metabolic garbage go that your brain cells produce? Where is the sewage system for the brain?
And she discovered it. It's actually made up of a set of cells called glial cells, which are these supporting brain cells. And so she called it the glymphatic system rather than the lymphatic system. So your brain does have its sewage system, this glymphatic system, and that's the discovery that she made. Remarkable.
Then, and I'm not quite sure what motivated her to do this, she started to measure how efficient that glymphatic, that waste system was when the rats were awake and when the rats were asleep. And what she found was that it's during deep sleep that these brain cells actually shrink by almost 60% when we sleep. Blows my mind.
Rhonda: Yeah.
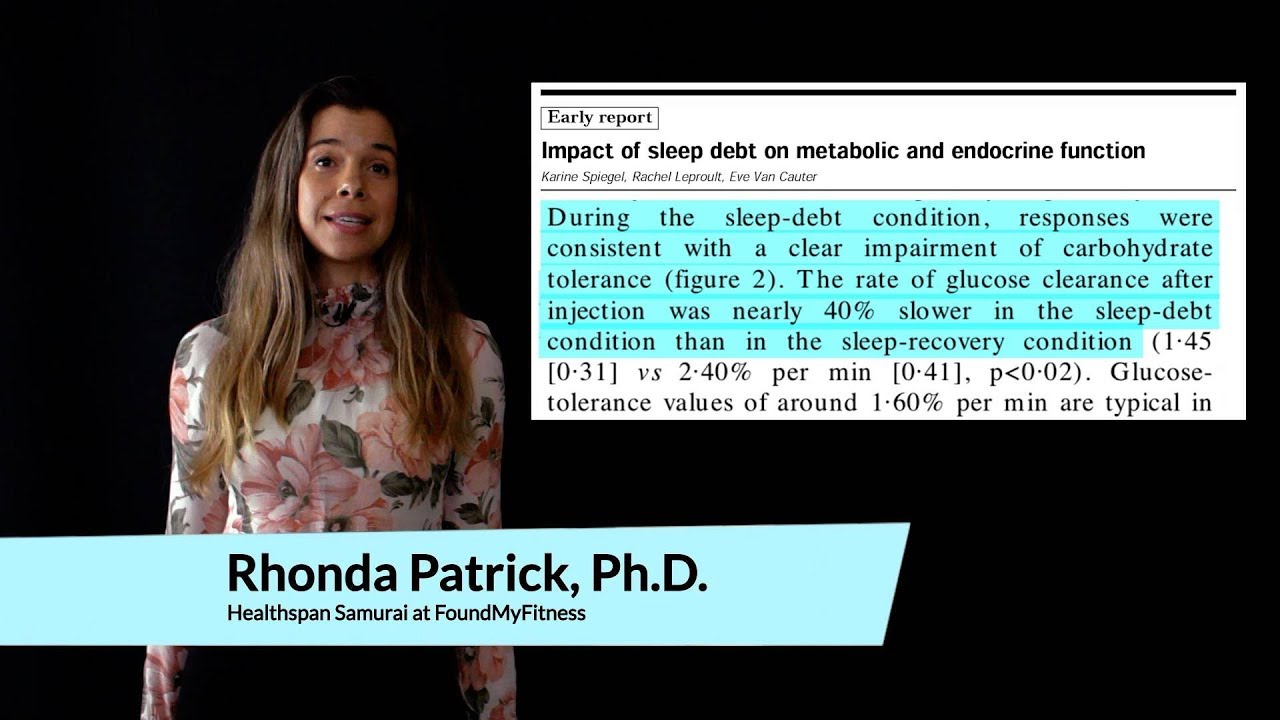
Matt: It's almost like, you know, all of the buildings in New York all of a sudden shrink, and it leaves these much greater, large areas for the cleaning crews to come in and clean up all of the metabolic detritus of the city's activity during the day. It's exactly what happens during sleep. And the cleaning solution is what we call cerebrospinal fluid. And through a pulsatile mechanism during sleep, you get a 10% to 20% increase in the bathing of cerebrospinal fluid through the brain, which washes away all of the metabolic byproducts that have been building up. One of those metabolic byproducts is beta amyloid. And, in fact, if you deprive those rats of that deep sleep, you immediately get an increase in toxic beta amyloid.
So now we've linked these two. I'm sorry it's a long story. But if you're not getting enough deep sleep at night, you're not giving yourself the chance for the kind of good night and sleep clean process to remove the beta amyloid. So more beta amyloid builds up. Where does it build up? Tragically, in the very same regions of the brain that generate the deep sleep that you need to clear out the toxic amyloid. So you start getting less deep sleep, so you get more toxic protein, more toxic protein, less deep sleep, less deep sleep. It's a self-fulfilling prophecy, and it's a nonlinear exponential curve.
If you look at how amyloid builds up in the brain, and if you look at the trajectory of Alzheimer's disease, it is a nonlinear exponential curve. It fits exactly what the sleep-dependent model of amyloid clearance would predict. If you're not getting sufficient sleep, that's the reason why now insufficient sleep seems to be one of the most significant lifestyle factors determining that.
Now you could say, by the way, those studies were in rats, and you deprived from the sleep for one night. What about humans? Like, surely...Well, the study has now been done. Great study done out of Wash U by a team of scientists led by David Holtzman. And they took a group of humans, and they did this very clever method where they deprive them of deep sleep but they didn't deprive them of sleep.
And you think, it sounds paradoxical. I can play you these auditory tones. Now this is not like the memory reactivation where you play a tone and then you leave the brain alone for a while. Here, I'm just going to keep playing tones to your brain, really sort of annoying tones. But I can play them at a level that doesn't wake you up, but it lifts you out of deep sleep and keeps you in shallow sleep.
So what's delightful about this method is that I can selectively excise one type of sleep, deep sleep, but I don't wake you up. So there's no stress of awakening. You are asleep for the same amount of time, but the quality of sleep is decreased.
Rhonda: Can street noise do that?
Matt: We don't know. Although I will come back to that when we speak about hopefully sleep appetite regulation, sleep glucose regulation, and sleep in low socio-economic cultures...
Rhonda: This is a little terrifying.
Matt: And I think that it's possible. I think there's other factors that link poor sleep in low SES, socioeconomic backgrounds. Is noise pollution one of them? I actually think it is. Untested as yet. But what they did with these human participants, they selectively remove deep sleep while keeping them asleep so total sleep time has not changed. And then, in the morning, they woke them up, they rolled them over, and they did a spinal cord puncture, a lumbar puncture, and they measured the cerebrospinal fluid that was percolating within the spinal cord, which also goes around the brain. And you can measure the amount of beta amyloid, which is a reflection of perhaps how much amyloid is there within the brain.
After one night of essentially a loss of deep sleep, you saw an immediate rise in the amount of beta amyloid. So it is a causal manipulation. That insufficient sleep in rodents and in humans will lead to a rise in beta amyloid.
Rhonda: Yeah. I think it was like 25% to 30%.
Matt: It was.
A neurodegenerative disorder characterized by progressive memory loss, spatial disorientation, cognitive dysfunction, and behavioral changes. The pathological hallmarks of Alzheimer's disease include amyloid-beta plaques, tau tangles, and reduced brain glucose uptake. Most cases of Alzheimer's disease do not run in families and are described as "sporadic." The primary risk factor for sporadic Alzheimer's disease is aging, with prevalence roughly doubling every five years after age 65. Roughly one-third of people aged 85 and older have Alzheimer's. The major genetic risk factor for Alzheimer's is a variant in the apolipoprotein E (APOE) gene called APOE4.
A toxic 42 amino acid peptide that aggregates and forms plaques in the brain with age. Amyloid-beta is associated with Alzheimer's disease, a progressive neurodegenerative disease that can occur in middle or old age and is the most common cause of dementia. Heat shock proteins have been shown to inhibit the early aggregation of amyloid beta 42 and reduce amyloid beta plaque toxicity [1].
One of three common genetic variants of the APOE (apolipoprotein E) gene. The APOE4 allele, which is present in approximately 10-15% of people, increases the risk of developing Alzheimer's disease and lowers the age of onset. Having one copy of E4 increases risk 2- to 3-fold, while having two copies increases risk as much as 15-fold.
Clear, colorless liquid present in the brain ventricles and the cranial and spinal subarachnoid spaces. CSF provides protection for the central nervous system and plays a prominent role in brain development and neuronal functioning. CSF is renewed about four times every 24 hours. Low CSF turnover rate, which occurs with aging, leads to accumulation of catabolites in the brain and CSF – such as amyloid beta – that are often observed in certain neurodegenerative conditions such as Alzheimer's disease.
A broad class of supportive cells in the central nervous system. Glial cells surround and provide support for and insulation between neurons. Unlike neurons, glial cells do not conduct electrical impulses. Glial cells are the most abundant cell types in the central nervous system, outnumbering neurons by a ratio of roughly 3 to 1. They are generally smaller than neurons, and they lack axons and dendrites. Types of glial cells include oligodendrocytes, astrocytes, ependymal cells, Schwann cells, microglia, and satellite cells.
A system that clears the brain of metabolites and other waste. The glymphatic system comprises a vast arrangement of interstitial fluid-filled cavities surrounding the small blood vessels that serve the brain. During sleep, these perivascular structures increase in size by more than 60 percent. This allows a “flushing” operation in which waste products can be eliminated. The glymphatic system also facilitates the distribution of essential nutrients such as glucose, lipids, and amino acids, as well as other substances, such as growth factors and neuromodulators.
The area of the brain located in the front portion of the frontal lobe, just behind the area commonly known as the forehead. The prefrontal cortex is involved in a variety of higher cognitive functions and behaviors such as executive function and expression of appropriate social behavior.
Good health. A person in rude health is full of vigor and free of illness.
A microtubule-bound protein that forms the neurofibrillary "tau tangles" associated with Alzheimer's disease. Tau tangles disrupt transport of metabolites, lipids, and mitochondria across a neuron to the synapse where neurotransmission occurs. Diminished slow-wave sleep is associated with higher levels of tau in the brain. Elevated tau is a sign of Alzheimer's disease and has been linked to cognitive decline.
Abnormal aggregates of hyperphosphorylated tau, a protein found in the brain. Tau tangles are associated with traumatic brain injury and chronic traumatic encephalopathy and are one of the defining characteristics of Alzheimer’s disease. They inhibit normal brain function, and the degree of cognitive impairment in diseases such as Alzheimer’s is significantly correlated with their presence.
Member only extras:
Learn more about the advantages of a premium membership by clicking below.
Supporting our work
If you enjoy the fruits of
 , you can participate in helping us to keep improving it. Creating a premium subscription does just that! Plus, we throw in occasional member perks and, more importantly, churn out the best possible content without concerning ourselves with the wishes of any dark overlords.
, you can participate in helping us to keep improving it. Creating a premium subscription does just that! Plus, we throw in occasional member perks and, more importantly, churn out the best possible content without concerning ourselves with the wishes of any dark overlords.
Sleep News
- Regular cannabis use during adolescence may be linked to long-term insomnia risk.
- People with insomnia benefit from regular mind-body or aerobic exercises, with yoga leading as the most effective—increasing total sleep time by nearly two hours.
- The air in children's sleeping areas harbors high chemical pollutant levels, potentially increasing young children's exposure to toxic compounds.
- Resistance training notably improves sleep quality in older adults, outperforming both aerobic and combined exercises.
- Sleep disruption reduces the newly discovered hormone 'raptin,' potentially increasing appetite and promoting weight gain.